Op-Ed: Do we have the will to stop TB?
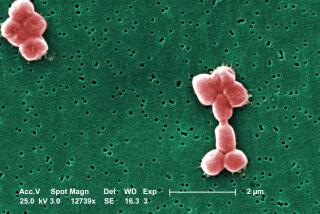
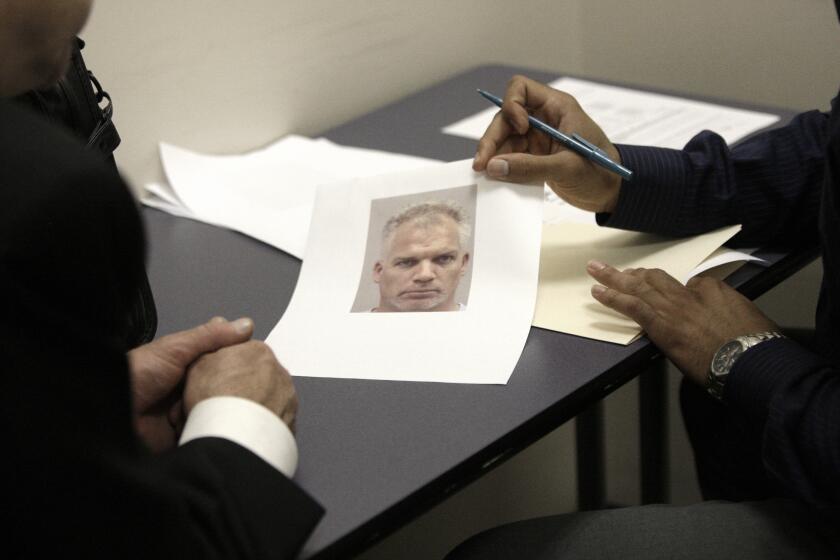
Doctors swear to do no harm, but I knew I was about to inflict great suffering on my patient Gary, who had been diagnosed with extensively drug-resistant tuberculosis, or XDR TB. Many people wrongly assume that tuberculosis has been eradicated. In fact, according to the World Health Organization, tuberculosis killed more people in 2015 than HIV/AIDS.
The strain affecting Gary is difficult to cure. Eighty percent or more of patients with XDR-TB die of their disease. There is grueling, toxic treatment available, but it doesn’t guarantee a cure. Gary would be facing permanent nerve damage. Constant nausea. Kidney damage. Hearing loss. He would have to take 10 to 12 drugs at a time for almost a year, and his follow-up treatment would last for another two years. He would have to spend nine months in deep isolation to prevent the spread of the disease. And he would have to lose a lung.
Drug-resistant TB is an individual tragedy, but it is also a public health nightmare.
Drug-resistant TB is an individual tragedy, but it is also a public health nightmare. At its worst, it has a prognosis similar to metastatic cancer, but it is transmitted through the air we breathe. The first signs of TB can seem mild — a fever, night sweats and, often, coughing. Later, unless proper treatment is given, TB kills. Patients undergo what feels like a slow drowning as the lungs fill with fluid.
The extreme form of drug-resistant TB that Gary had is fortunately still a rare disease in the United States, but it develops from a more common form, called multi-drug resistant tuberculosis — MDR TB. This form too requires a complicated and toxic treatment regimen similar to XDR TB. The cost of treating either strain is enormous: an estimated $400,000 per case of MDR TB and $1 million per case of XDR TB.
Both XDR and MDR TB spring from the same roots: inadequate treatment for regular TB, which is often the result of weak public health systems around the world. Patients don’t get treated because they or their doctors think they have another illness. Stigma can lead to a delay in seeking care. In some countries, there are few labs that can determine which medicines will work best, so doctors guess. And although treating regular TB is easier than the drug-resistant kind, it is still long and difficult, and the treatment must be strictly adhered to or the bacteria won’t be wiped out.
All of this means that the TB has ample opportunity to develop resistance to the drugs used to treat it. Once resistance takes hold, that strain can spread and it becomes even harder to cure.
In the United States, there are more than 9,000 cases of regular TB and about 100 new cases of MDR TB a year. California leads the nation in new cases of MDR TB, with 30 cases last year and 20 documented so far this year. We see more of the disease because we are a gateway state, with people coming here to live, work or study from countries, often in Asia or Eastern Europe, where drug-resistant TB is more common. Globally, there were an estimated half a million new cases of MDR TB in 2014; perhaps a quarter of them were diagnosed and treated, and only half of those were cured.
It’s a bleak picture, and one that could get worse. In his 2016 budget, President Obama proposed a cut of $45 million in funding for global TB programs. However, earlier this year, the White House also announced the development of an “action plan” to stimulate drug-resistant TB research and treatment at home and abroad. The president should request the funding required to implement the plan.
TB anywhere is a threat everywhere. It can be cured, and even the drug-resistant varieties can be stopped. Gary is in his second year of treatment. It’s been arduous; he requires oxygen because he now has only one lung. He has painful nerve damage in his hands and feet, and he’s nearly deaf. But he is no longer infectious, and he is alive.
There will be those who say we can’t afford comprehensive action to stop tuberculosis. But when we consider the suffering of patients like Gary, and the danger to us all, how can we afford not to?
Dr. Caitlin Reed directs the Inpatient Tuberculosis Unit at Olive View-UCLA Medical Center. She is an assistant professor of infectious diseases at UCLA’s David Geffen School of Medicine.
Follow the Opinion section on Twitter @latimesopinion and Facebook
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.