How to sort through new health plans
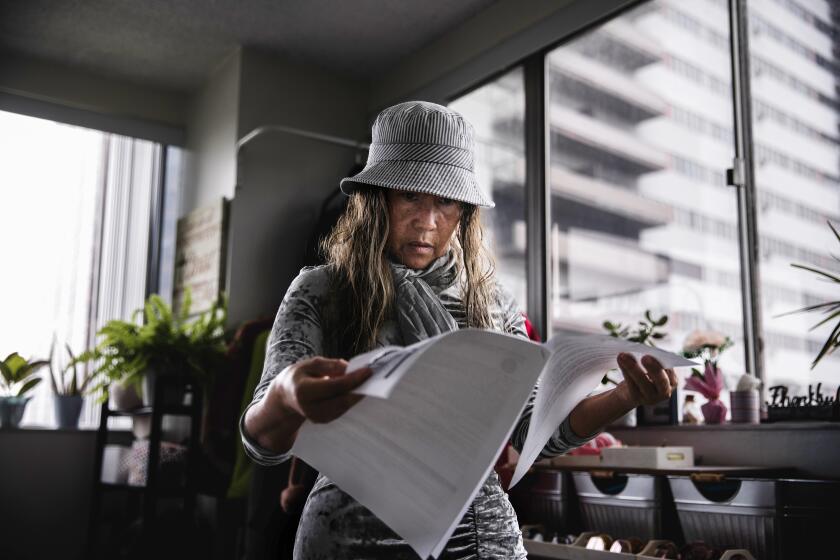
Mike and Annette Heacox, married for 23 years, run a landscape architecture firm in Sacramento. For the last 14 years, they’ve bought their own health insurance — most recently a small-business policy bought through a local insurer.
Now — with health coverage on everyone’s minds — the couple are in the market for a new health plan, and they’ve embarked on a confusing trip through the world of insurance.
While navigating their way through various options, one thing was clear to Mike Heacox: The price was right. “For us it’s a no-brainer,” he said. “We’d save a lot of money over our current premiums.”
But many questions remain for consumers like the Heacox couple as they sort out health plan options. Here is a snapshot of what experts say they should consider.
Small-business vs. individual and family policies
The couple said they have poked around on Covered California, California’s health insurance exchange, but haven’t yet gone through the process of signing up for coverage.
Covered California’s home page left Mike Heacox scratching his head; right away he had to decide if he was an individual — or a small business.
“I went to enroll and I was like, now I have to know if I’m going to go through the business or not — and I got stopped because I don’t know,” he says.
There are many factors for small businesses to consider in shopping for policies — including trying to decide whether their employees would be better off getting insurance at work or applying on their own through the exchange.
But the Heacoxes, as strictly a husband-and-wife business, ran into a different problem. It turns out they are among roughly 500,000 couples in California who are no longer eligible for small-business policies like they have had in the past. To be eligible for a small-business health insurance policy, “you have to have at least one employee that is not related,” says Anthony Lopez, small-business specialist with online health insurance broker eHealthInsurance.
That means the couple will need to drop their current small group plan and search for family coverage.
Anticipating fluctuating income
It’s a family’s annual household income that determines eligibility for subsidies when buying insurance through Covered California.
This can be tricky for freelancers and small-business owners like the Heacoxes who don’t have regular paychecks and often don’t know what next year’s income will be.
“We don’t have a way of saying what we’ll make every year or even every month, so we just don’t know,” Annette Heacox says. The couple have seen major ups and downs in income during the recession and since then, she said.
According to Ken Jacobs, chair of the Center for Labor Research and Education at UC Berkeley, people in the Heacoxes’ situation should report an average of their income in recent years when applying for insurance.
“People should be conservative in their estimates,” he said, to avoid having to repay the subsidies they received.
“If your income changes, that should be reported right away,” Jacobs says. “Doing so makes a very big difference in what people can owe at tax time.”
Cost savings on the horizon
The Heacoxes currently pay $1,100 per month for their health insurance. A search on Covered California’s website shows that a mid-level Silver plan could save the couple as much as $900 per month.
Plus they’ll get a break on costs each time they visit the doctor or pick up a prescription.
But price isn’t everything, says Bruce Benton, executive vice president of the insurance agency Genesis Financial and Insurance Services. He advises consumers to look deeper into what each plan covers and whether their doctors are included in the network.
Exchange vs. Medi-Cal
Individuals earning up to about $46,000 and families earning up to $94,000 are eligible for subsidies when they buy a health insurance plan through the exchange. But for lower-income people, there is the state’s Medi-Cal program, which has no monthly premiums.
Should business once again begin to slow for Mike and Annette Heacox, and their income drops to where it was in 2010 and 2011, the couple could qualify for Medi-Cal coverage.
“People on the income threshold could easily, in any given year, flip between Medi-Cal managed care and the exchange,” says Dylan Roby, director of health economics and evaluation research at the UCLA Center for Health Policy Research.
To avoid disrupting their relationship with their doctors and their health plan, Roby suggests customers like the Heacoxes choose an insurer that offers both Medi-Cal and exchange plans, if possible.
Although the networks are often different between Medi-Cal and exchange plans — even when offered by the same insurer — sometimes there is overlap.
That way the only thing that changes, Roby says, is “once they cross that eligibility threshold into the exchange from Medi-Cal they start paying their own premiums.”
Resources and links
Here are a few websites to explore your options:
California’s Health insurance exchange: https://www.CoveredCA.com
To find Health insurance exchange information outside of California: https://www.Healthcare.gov
To find an insurance agent certified to sell plans through the marketplaces: https://www.nahu.org/consumer/findagent2.cfm
Zamosky writes about healthcare and health insurance. She is also the author of a new book, “Healthcare, Insurance and You: The Savvy Consumer’s Guide.”