Genetics to determine cancer treatments
The war on cancer is poised to enter a new phase that promises more precise treatments, fewer side effects and, most of all, more survivors.
And none too soon. Although death rates from many cancers have slowly but steadily declined over the decades, experts agree that current treatments are mostly too blunt, too scattershot and too dangerous for the patients they are intended to save.
Today, treating cancer often means an all-out chemical assault on tumors. Doctors bombard patients’ bodies with drugs that aim to destroy cancer cells. But like shelling an entire city to wipe out a few rebels, the strategy leaves civilian casualties in its wake: Standard cancer treatments destroy healthy cells alongside diseased ones, taking a toll on a patient’s body and strength.
Now, however, the battle tactics are shifting. Researchers have learned how to gather intelligence on a cancer’s traits, turn off the tumor’s defenses and precisely target only the cells that are causing disease.
“We have the confluence of all these advances coming together at once,” says Dr. Ronald DePinho, president of the University of Texas MD Anderson Cancer Center in Houston. “I’m not saying we can cure cancer within 10 years. But we’ve been handed a complete toolbox. Within this decade, there’s no question that we’re going to accelerate the decline in mortality due to cancer.”
DePinho says the recent revolution in genetics has reignited the world of cancer research. Scientists can sequence all the genes in a cancer cell faster than ever before, compare the cancer genes with those in the rest of the body and even turn genes on and off.
Using these technologies, researchers have discovered that similar-looking cancers can have very different genetic makeups. Understanding the world of mutations can help doctors predict how quickly cancer will grow and which drugs will kill it.
“Oncology as a discipline has always divided itself around body sites,” says geneticist Elaine Mardis of Washington University School of Medicine in St. Louis. “There are people who focus on lung cancer and people who focus on breast cancer and people who focus on pancreatic cancer.” But the field has realized that cancers are defined as much by their genetic mutations as by location, she says.
When new cancer drugs are in clinical trials, it’s already standard practice to see whether the patients who respond have any telltale genetic markers. And in some, cases, such genetic signatures have been found.
Last year, the Food and Drug Administration approved vemurafenib, a melanoma drug that works only in patients with a particular mutation in a gene called BRAF. The drug has no effect in patients without the mutation, so a genetic test is required before a doctor can prescribe it.
DePinho says that decoding the genetics of patients and their tumors will help doctors choose drugs that can target the disease most effectively and with the fewest possible side effects.
“Understanding a person’s genetic profile allows us to perform precision medicine,” he says. “It’s absolutely clear that all cancer patients will receive genetic profiling in the not-too-distant future.”
While the BRAF gene test requires a sample of tissue from a tumor — easier for a skin melanoma than for cancers deep within the body — future tests could rely on something even more routine: a vial of blood.
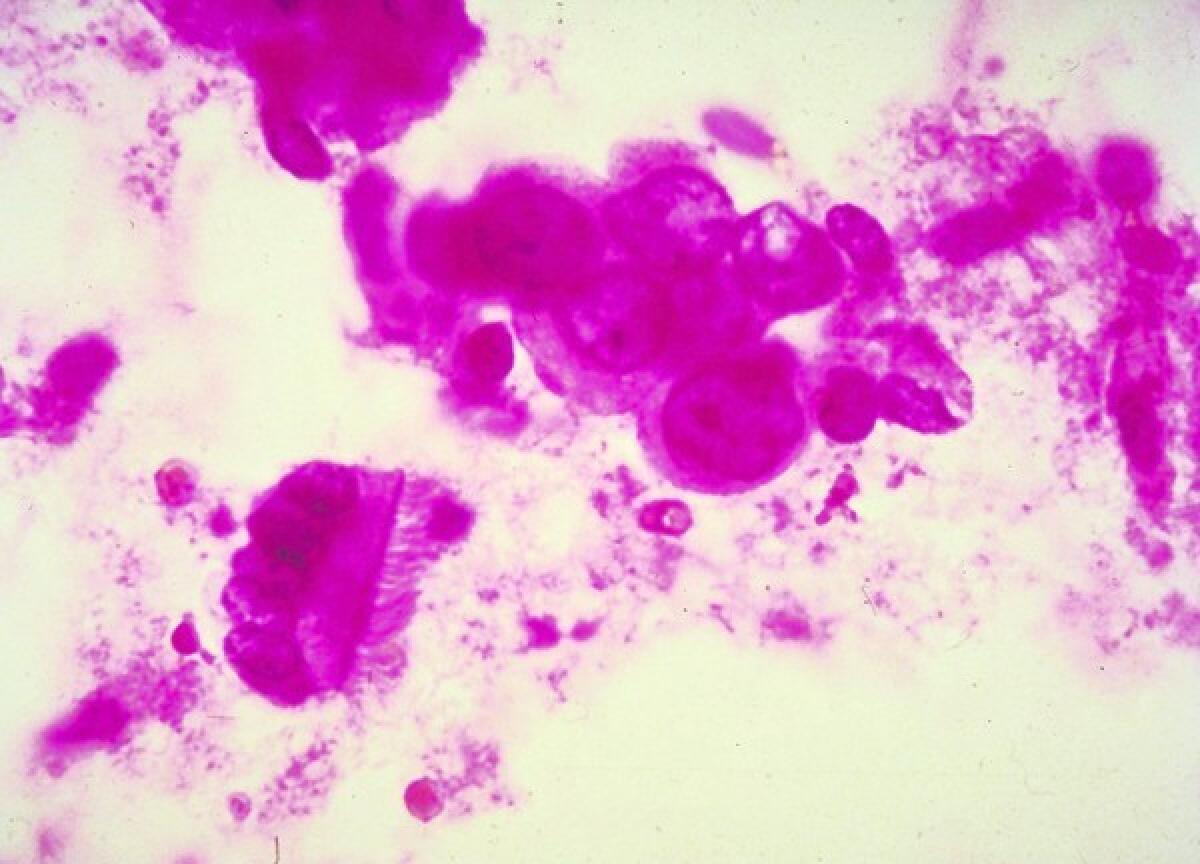
At Scripps Research Institute in La Jolla, researcher Peter Kuhn and his colleagues have developed a “fluid biopsy” that can examine tumors through a simple blood test. Tumors are constantly shedding loose cells into the bloodstream — it’s how cancers can spread to new areas in the body. The researchers have found that they can isolate the cells and study their genetics without making a single incision.
“Five years from now, every time a patient with a solid tumor walks into the doctor’s office and blood work is being done, a tube will be drawn for a fluid biopsy,” Kuhn says. “Ten years from now, I think we ought to be beyond cancer patients and also be testing people at high risk for cancer.”
As fluid biopsies become more routine, he says, researchers will have a wealth of data — sampled repeatedly throughout a patient’s illness — that can guide the course of treatment. It will be one more way to personalize the war against cancer.
The future of cancer also means new approaches to treatment. Since cancer cells often have unique properties that set them apart from healthy cells, researchers are coaxing the immune system to find the cancer cells and mark them for destruction. The approach is called immunotherapy, and it has many researchers excited.
“Immunotherapy offers the hope of targeting cancer cells very specifically without damaging normal, healthy cells,” said Dr. Jeffrey Miller of the University of Minnesota, who studies one type of immune cell. “These types of agents are dramatically changing the repertoire of possibilities for treating cancer. We’re way more optimistic today than we were 15 years ago.”
Of course, before any of these tests and treatments can make a difference in patients’ lives, they need to make it through clinical trials and win federal approval. But the drug approval process still revolves around the old thinking of cancers as defined by location. That will have to change, experts say.
“If a drug goes through clinical trials in lung cancer, then it’s approved for lung cancer. And insurance companies won’t pay for off-label use, so it will only be prescribed for lung cancer,” Mardis says. As doctors and scientists continue targeting tumors all over the body, the approval process will have to evolve, she adds.



