With HIV, growing older faster
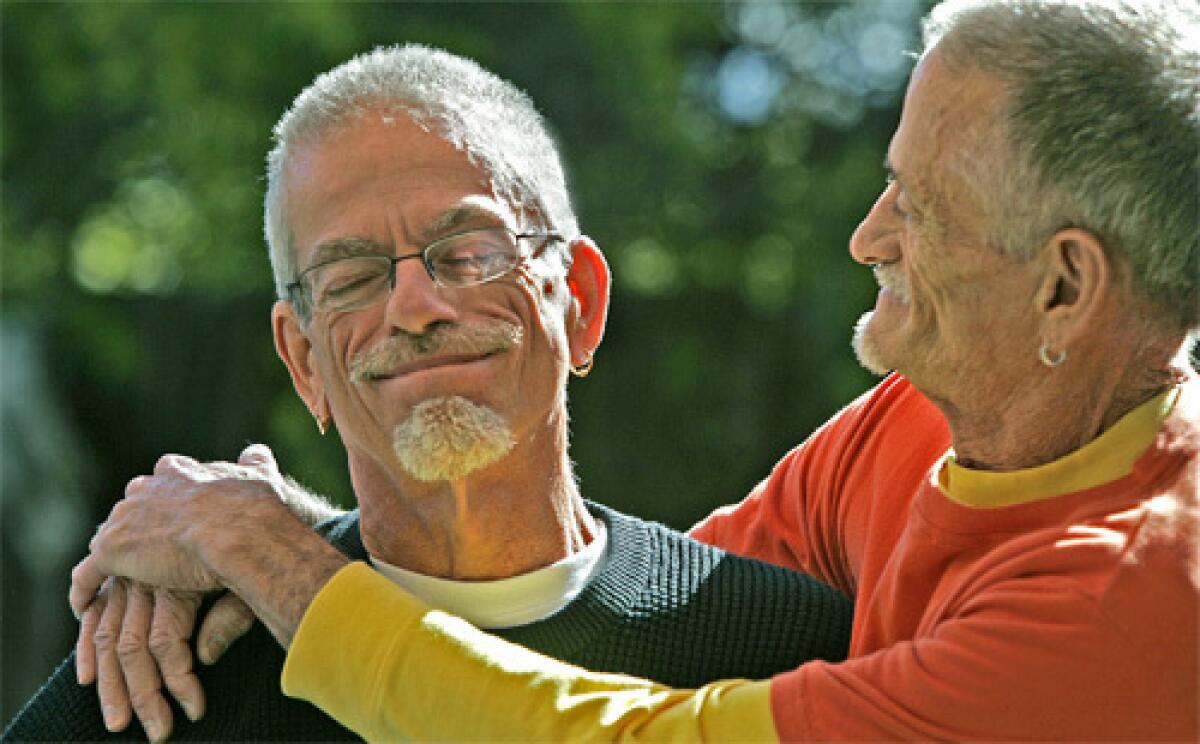
Larry Gibson first spotted Dennis Golay outside West Hollywood’s French Market Place. By the time he was halfway across Santa Monica Boulevard, he’d fallen in love.
It was Nov. 14, 1981 -- Golay’s 34th birthday.
Seven years later, both men tested positive for the AIDS virus, an almost certain death sentence in the days before antiretroviral drugs. Having dreamed of growing old together, they were devastated.
“We had something so special,” said Gibson, 63, looking back at that dark time. “To be cheated out of its maturity just didn’t seem right.”
“I guess it wasn’t,” said Golay, now a silver-haired 60. “We’re still here.”
Much attention has been paid in recent years to how the human immunodeficiency virus disproportionately infects African Americans and Latinos, including women, many of them poor. But the new reality of HIV is not just black or brown. It is also gray.
The graying of HIV/AIDS is a little-recognized new phase of the epidemic in the United States, and it comes with its own complications. Gibson and Golay are growing old together, true. They are also growing older faster. Ailments common to aging, including depression, are showing up sooner than expected in many people with HIV, according to patients and the doctors who treat them.
“We’re seeing things that my mother is experiencing,” Golay said, “and she’s 86.”
Golay had a heart attack last year at 59, despite a lifetime of healthful eating and regular exercise. He underwent a quintuple bypass. (“He never does anything small,” Gibson said.) His father had died of a heart attack -- at 70.
Gibson has the sunken eyes and cheeks of an old man, side effects of the antiretroviral drugs that keep his HIV in check. Lipodystrophy, as the condition is called, rearranges fat in the body and at one point gave Golay a humped back. It can lead to insulin resistance and raise cholesterol and triglyceride levels in the blood.
Lethal infections
Some longtime survivors develop a bone disease possibly linked to the use of corticosteroids against pneumocystis pneumonia, one of the most lethal of the opportunistic infections that prey on HIV-weakened immune systems. Called avascular necrosis, the bone disease can lead to the need for a hip replacement. Others aging with HIV are developing memory deficits and liver and kidney diseases.
“I have a population that, having survived this terrible illness, is now getting illnesses of old age 10 or 20 years sooner than normal,” said Dr. Ardis Moe, a physician at UCLA’s Center for Clinical AIDS Research and Education. “That’s the bad news. The good news is that they’re not dead.”
Early on in the epidemic, the quickly mutating virus developed resistance to the first drugs found to suppress it. Then, in 1996, researchers discovered that multi-drug “cocktails” of three antiretroviral drugs were better barriers to mutation than single drugs. Deaths plummeted.
Today more than 25 anti-HIV drugs are on the market, allowing numerous combinations to combat resistance and adjust for side effects. But health problems persist, and doctors have few guidelines for teasing out which conditions are caused by the virus, which are side effects of medications and which are merely signs of aging.
Until the last decade, there were too few people aging with HIV to study.
Now more than a quarter of the estimated 1 million Americans living with HIV are, like Gibson and Golay, older than 50, according to the federal Centers for Disease Control and Prevention. By 2015, half will be older than 50. At least two long-range studies of people aging with HIV are underway, by the National Institutes of Health and the Veterans Health Administration.
A 2006 study by the New York-based AIDS Community Research Initiative of America on the interaction of HIV and aging on mental health found depression to be almost 13 times higher in longtime survivors than in the general population. As do the very elderly, whose suicide rate is the highest of any age group, longtime HIV survivors often grow despondent over health disabilities and the deaths of friends.
“Everybody I knew died in the late ‘80s or early ‘90s,” said Los Angeles resident and longtime survivor Thomas Woolsey, 59. “It sounds like I’m the lucky one, but I don’t really think so. What good is a life without any friends?”
Feeling invisible
When AIDS Project Los Angeles started a support group for people over 50 last fall, Woolsey became a regular. “I go not so much for therapy but to see human beings,” he said.
Feeling invisible is common for those with HIV, whether longtime survivors or recently diagnosed, said therapist Richard Levin, who runs the group.
“It’s common in aging,” he said. “And it’s common in the gay community, especially in Southern California, where youth and being new and vibrant are valued.”
In few places is the graying of HIV as evident as in Palm Springs, the gay-friendly vacation and retirement hub. At the Desert AIDS Project, a medical and social services agency in Palm Springs, 40% of the 2,300 clients are older than 50.
Bill Cooksley is one of them. Today a fit 71, he was 66 when he became infected with HIV. He almost died -- of shame.
“For a week after I was told, I isolated myself completely,” he said. “I felt so stupid. It was my own damned fault. How could I tell anybody?”
A community college counselor and instructor in San Diego, Cooksley had retired to Palm Springs in 2000. He’d spent decades being careful. Then one time, he was not. A combustible mix of relief and disbelief that a younger man found him desirable triggered the lapse.
His euphoria was as fleeting as the relationship. A multi-drug cocktail kept his HIV in check, but it couldn’t touch his depression. He weighed suicide.
A Desert AIDS Project support group and daily gym workouts got him out of his house and saved his life, he said.
Making an effort to “engage in life,” said Gibson and Golay, also saved them after they moved to Palm Springs years ago, expecting to die.
When the two men met, whispers of a mysterious “gay cancer” circulated within L.A.’s gay community. By 1983, their friends were dying in droves.
Together for two years by then, they thought at first that they’d dodged the bullet. Then Golay learned that a former boyfriend had died of AIDS. A few years later, Gibson saw his former partner’s name on a panel in the AIDS Memorial Quilt, the patchwork tribute to those who’d been lost to the epidemic. They now believe that each of them was infected before they met.
After testing positive, they formed a pact:
They would not assign blame.
They would do anything they could to survive.
They would help everybody who needed help.
Doctors gave them 18 months to live. A year passed, then two. They sold their Silver Lake house with its bubble-gum pink door and moved to Florida to be closer to Golay’s mother. Closeness, they learned, had its limits. On a solo drive west to find a new home in Los Angeles, Gibson stopped in Palm Springs. Once again, it was love at first sight.
They had other reasons to leave Florida: The two men were getting sicker, and HIV care there was “dismal,” Golay said. Not so in Palm Springs, where the Desert AIDS Project had established itself as one of the most comprehensive medical and social service agencies in the country.
The couple bought a tiny box of a house with bare sand for a yard and made it into a desert oasis. Gibson built the cabinets in the galley kitchen. Golay planted palm and fruit trees. They planned for the worst but hoped for the best.
By 1996, hope was getting harder to come by. Gibson went blind in one eye from an opportunistic infection. At one point, he had just 16 T cells -- which normally orchestrate the body’s immune response -- per cubic millimeter of blood.
Healthy people have from 500 to 1,600.
“We decided that if they got below 10, we would name them,” Golay said.
That was the year Gibson was selected for a clinical trial of the first of the antiretroviral drugs that ultimately reclaimed so many lives. Within three weeks, he began to gain strength.
Still, there were setbacks.
When Gibson entered the clinical trial for the anti-HIV drugs, he found out that he was also infected with hepatitis C. Last year, in an unsuccessful bid to rid himself of that infection, he underwent a harrowing round of chemotherapy, then got even sicker when one of those drugs conflicted with his HIV medication.
Gibson and Golay are not complainers by nature. Part of their pact -- to help everyone who needs help -- includes taking part in drug trials even if benefits come too late for them.
It also means sharing the philosophy that has seen them through the worst of the epidemic and each new challenge.
“All you can do is treat the problem in front of you,” Gibson said. “We adjust. We adapt.”
They are the oldest surviving couple they know.
“We’re old-timers now,” Golay said. “We’re a resource for people. That’s kind of gratifying. It’s one of the good things about getting older.”
More to Read
Start your day right
Sign up for Essential California for news, features and recommendations from the L.A. Times and beyond in your inbox six days a week.
You may occasionally receive promotional content from the Los Angeles Times.






