3 King/Drew Deaths Blamed on Lapses

Over the course of four days late last month, three more patients died at the beleaguered Martin Luther King Jr./Drew Medical Center after what officials believe were critical lapses in care.
A Los Angeles County coroner’s report attributes the death of one patient, Robbie Toney, to complications from the placement of her breathing tube, which caused her lung to collapse. The coroner said the March 25 death of the woman, 61, was from a medical accident, not natural causes.
For four hours before her death, Toney had complained about pain where the tube had been inserted, county health officials said this week. They are investigating whether doctors and nurses at the county-owned hospital failed to recognize that the pain was a sign of trouble and whether the tube had been placed properly in the first place.
Toney’s daughter, Marshon, said Tuesday that no one at the hospital had informed her of any potential problems with her mother’s care. A King/Drew official simply asked if an autopsy could be performed, she said.
“I’m very startled and dumbfounded and overwhelmed now,” she added.
Toney’s death and those of the other two followed months of public assurances by county officials and King/Drew managers that employees had been rigorously retrained and new policies put in place to prevent breakdowns in care.
Yet the errors involved in the deaths mirror those that regulators, accreditors and even the outside consultants running the hospital have repeatedly cited in the last year.
In at least two of the cases, including Toney’s, county health officials say it appears that doctor trainees did not receive appropriate oversight from more-senior physicians, as required. The hospital has often been faulted for failure to supervise doctors training to be specialists.
The county Board of Supervisors, which has drawn criticism for its timidity in tackling King/Drew’s woes, discussed the deaths in closed session Tuesday but took no formal action.
Four supervisors — Zev Yaroslavsky, Gloria Molina, Don Knabe and Mike Antonovich — either declined to comment or did not return phone calls after the meeting.
Supervisor Yvonne Brathwaite-Burke, whose district includes King/Drew, said she did not know what effect the deaths would have on the hospital’s future because it was being scrutinized so intensely.
“They’re under the microscope,” she said, “so anything certainly causes concerns.”
According to the county’s preliminary investigation, the recent incidents also included:
A critically ill man with AIDS who died March 27 after King/Drew staff inexplicably waited seven hours to transfer him from a medical ward to the intensive-care unit.
County Department of Health Services officials expressed concern in a memo to the supervisors late Monday that the appropriate staff was not attending the patient during the transfer, when he went into cardiac arrest and could not be revived.
A patient with liver disease, who died March 28 and may not have received the appropriate medication at the right times for low blood pressure. The memo also said an anesthesiologist did not respond to a Code Blue alert, as required.
Each of the three patients was seriously ill, and it is not clear how long they would have lived without the lapses, county officials said.
But in its memo, the health department said the care of all three patients “did not meet the community standard.”
“We’re all disappointed when we find another episode that is unexplainable, where errors in judgment and failure of supervision happen when we have really identified all the problems,” said Dr. Thomas Garthwaite, health department director, in an interview.
Marshon Toney said her mother had moved back to Los Angeles, where her family lives, in December.
Robbie Toney was quite ill and had only months to live, coroner’s records show. But during the 18-day hospital stay, Marshon Toney said, doctors told her mother that she might be able to go home with a ventilator.
The daughter said she got an urgent call March 25 that her mother had taken a turn for the worse. When she arrived at King/Drew, staffers took her to a room and told her that her mother had died.
“I didn’t question it, because she was really ill,” the younger Toney said. “At the time when I’m looking at my mom’s freshly dead body in the hospital, I’m not thinking” that any mistakes might have been made.
Garthwaite said he did not know if patients’ families had been told about the problems with the care.
In a five-part series in December, The Times identified several instances in which the hospital failed to tell patients and their relatives about serious lapses in care, even when doctors knew about them.
The deaths again highlight systemic breakdowns at the hospital in Willowbrook, south of Watts. County officials this week said they were troubled by similarities between the recent failings and those detailed only three months ago in a 1,000-page report by Navigant Consulting Inc.
The firm, which took over the hospital’s operations Nov. 1 under a yearlong $13.2-million contract with the county, has said some of the problems are already fixed.
For example, in January, Navigant found that anesthesiologists were not showing up for Code Blue emergencies unless others summoned them.
At a public meeting in February, Navigant director Kae Robertson told county supervisors that anesthesiologists would henceforth respond to the alerts. Although county officials say the lack of an anesthesiologist did not cause the liver patient’s death, the failure to respond is troubling, given the prior promises, said Fred Leaf, the health department’s chief operating officer.
Doctors at King/Drew, through their attorney, released a statement saying Navigant had not distributed needed pagers to doctors that would alert them to Code Blues.
“There were ample physicians present in the hospital to respond to the Code Blue,” said attorney Mark Ravis, who is suing the county over King/Drew cutbacks. “It is not their fault that Navigant hasn’t gotten around to distributing the pagers.”
Robertson would not comment on the individual patient cases or the pagers. Navigant has made it “pretty clear” that anesthesiologists are expected to respond to Code Blues, she said.
“There is a policy. It’s been agreed to. It’s been disseminated, and there’s a way that they are reached,” she added.
Problems with medication administration have been even more pervasive for more than a year. In March 2004, government health inspectors found that staff repeatedly withheld medications from patients and administered the wrong drugs or dosages, in some cases even as the inspectors looked on. As a result, the medical center almost lost its federal money.
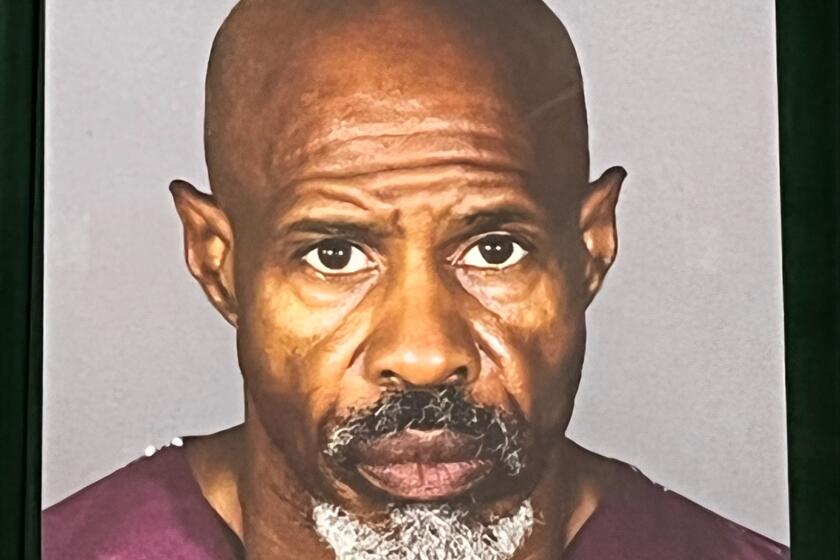
Similarly, regulators and even hospital administrators have accused King/Drew and its affiliated medical school of a lack of physician-trainee oversight. In January, for instance, Dr. Roger Peeks, the hospital’s medical director, sent out a memo saying “inadequately trained and not properly supervised” first-year residents inadvertently left guide wires in three patients.
Federal health officials, who have been closely monitoring care at King/Drew, say they are waiting for the hospital’s final analysis of the deaths before deciding how to proceed.
“At this point it seems that there was some less-than-ideal care being provided to these people,” said Steven Chickering, a regional official with the U.S. Centers for Medicare and Medicaid Services.
“But we don’t have all of the facts at this point,” he added. “We’re going to let them complete their investigation and provide that information to us. We’ll analyze that, and then we’ll decide what our next step will be.”
Garthwaite said that King/Drew and county officials could change systems and discipline staff but that good care depended on individual nurses and doctors.
“There are still additional members of the attending [physician] staff who don’t get the seriousness of this,” he said. “We still need to identify those individuals and move them out.”
More to Read
Start your day right
Sign up for Essential California for news, features and recommendations from the L.A. Times and beyond in your inbox six days a week.
You may occasionally receive promotional content from the Los Angeles Times.