Healthy? Insurers don’t buy it
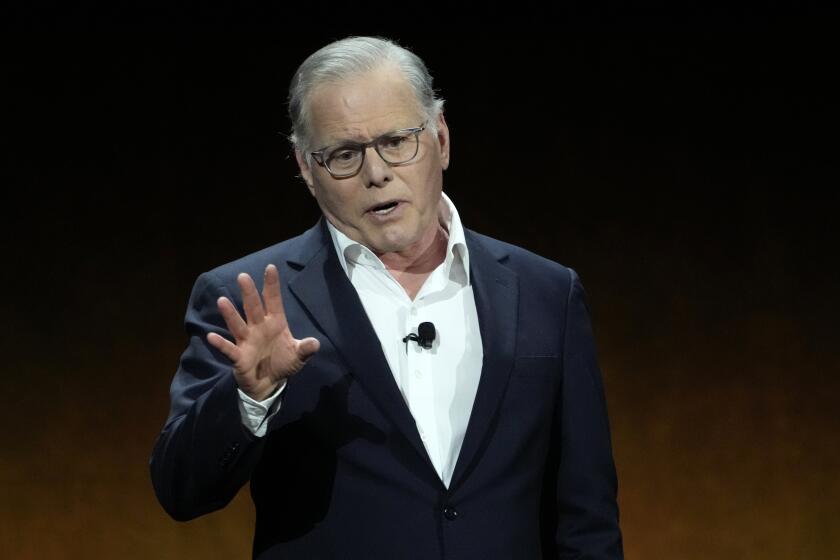
Scott Svonkin joined the Los Angeles County Commission on Insurance 10 years ago because he was concerned about an emerging problem: people losing health coverage. Since then, the ranks of uninsured Americans have swelled to more than 46 million.
Svonkin almost became one of them.
It happened after he left a comfortable government job as a legislative chief of staff to start his own marketing and public affairs consulting business. Late last year he started shopping around for health insurance for himself, his expectant wife and his young daughter.
He knew he’d pay more without an employer picking up most of the tab. And he knew he’d have to fill out a medical questionnaire because, unlike job-based coverage, individual insurance in California is contingent on an applicant’s health. But that didn’t concern him because, he said, “I’m healthy as a horse, never smoked and have had no major surgery.”
As it turned out, Svonkin was rejected by not just one but three of California’s biggest health insurers, which cited his history of asthma, among other things.
“I couldn’t buy it at any price,” said Svonkin, 40, who lives in Sherman Oaks. “I remember thinking, ‘This can’t be happening to me.’ ”
Svonkin is part of what experts say is a largely hidden aspect of the nation’s health insurance crisis: the uninsurables, people whom insurance companies won’t touch, even though they can afford to pay high premiums. Some, such as Svonkin, pay steep rates for lean coverage from the state’s high-risk insurance pool. Others simply go without.
Insurers have wide latitude to choose among applicants for individual coverage and set premiums based on medical conditions. Insurers say medical underwriting, as the selection process is known, is key to keeping premiums under control.
“Our goal is to extend affordable coverage to as many people as we can,” said Cheryl Randolph, a spokeswoman for PacifiCare Health Systems Inc., a subsidiary of Minneapolis-based UnitedHealth Group Inc. “But because of the medical underwriting, we do not accept everybody.”
Selective insurers
Consumer advocates see the practice as cherry-picking -- a legal form of discrimination that is no longer tolerated in schools, public accommodations or workplaces -- and a way to guarantee profits.
“The idea is to avoid all risk,” said Bryan Liang, executive director of the Institute of Health Law Studies at California Western School of Law in San Diego.
Jerry Flanagan, an advocate with the Foundation for Consumer and Taxpayer Rights, said it wouldn’t take much to be left out of the private-insurance market. “A minor asthma condition or a surgery 10 years ago that requires no further medical care is enough to get you blacklisted forever,” he said.
As a result, some people forgo treatment so as not to tarnish their health records. Others withhold information from doctors or ask them to leave details out of their records. For those who are uninsurable, healthcare often is the chief reason they stay in or take a certain job.
Claudine Swartz enjoyed running her own consulting business but had been rejected for individual insurance. After a scare over a benign cyst in her breast, the San Francisco resident closed her business and got a job with the University of California’s health system, where she enjoys guaranteed coverage.
The episode made her realize that without insurance, she would have been on the hook for catastrophic expenses if her diagnosis had been more serious.
“I wasn’t willing to take that risk,” said Swartz, 35. “It’s a real problem for people trying to be entrepreneurial and work on their own.”
Uninsurable individuals pose a significant challenge for the state, which expects to spend more than $10 billion this year on people who lack adequate coverage.
Gov. Arnold Schwarzenegger, preparing to announce a proposal for expanding coverage in his State of the State address, has said he favors a mandate on individuals to buy health insurance -- just as drivers must carry auto insurance.
Democrats, who control the Legislature, have favored expansion of employment-based insurance and have signaled their opposition to a mandate on individuals.
Consumer advocates say such a mandate is unworkable unless insurers are required to sell coverage to all comers, as they are in several states, including New York and Massachusetts.
No one knows how many Californians are uninsurable. Blue Cross of California, which dominates the market, declined to disclose its rejection rate, as did its chief competitors. A 2004 industry survey found that health plans said they turned away about 12% of all applicants. But the rejection rate rose with age to 30% for people 59 and older.
A consumer survey this year found that 1 in 5 people who applied for individual coverage was turned away or charged a higher premium because of preexisting conditions. Experts say it is hard to know how many of California’s more than 6 million uninsured residents are uninsurable because many people with medical problems don’t even bother applying in the belief that they would be rejected.
Insurers tread carefully
The industry contends that individual coverage is widely available. But experts say a wave of consolidation has reduced the number of insurers offering individual coverage, leaving a marketplace that shuns all but the ostensibly healthiest consumers.
Insurers say they are picky because they have to be.
Kaiser Permanente’s “fairly generous” benefits require that the health maintenance organization be restrictive to remain solvent, spokesman Jim Anderson said. “We have to be very careful to not enroll a bunch of people who are going to spend all the money on their care.”
Insurers declined to disclose the underwriting guidelines that lead to rejection or higher premiums. But a review of public records, as well as rejection letters sent to individuals, shows that California carriers turn people away or charge them higher premiums for conditions that range from the catastrophic to the common. Cancer, epilepsy and AIDS make the list, along with breast implants, ear infections, varicose veins and sleep apnea.
Jeffrey Miles, a vice president of the California Assn. of Health Underwriters, a trade group for independent insurance agents, said one of his clients -- a 27-year-old woman “in perfect health with absolutely nothing wrong” -- was rejected because she had seen a psychologist for three months after breaking up with a boyfriend.
“I call it hangnail underwriting,” Miles said. “If a person has taken virtually any medication, they are going to be turned down. If people have had any psychological counseling at any time in recent history, they are going to get turned down.”
Swartz, the consultant, said the reason she couldn’t get individual coverage was a condition in her records that she may never have actually had. Her physician had diagnosed ulcerative colitis. But after years without additional symptoms, Swartz said, her doctor decided the initial diagnosis was probably wrong.
Consumer advocates say out-of-date, ambiguous and even erroneous medical information can render people uninsurable. Sometimes the reasons can seem absurd. In a letter to an otherwise healthy recent college graduate, for instance, Blue Cross listed among the reasons it denied coverage a past bout of jock itch, “successfully treated with cream.”
A last resort for people turned away by the private market is the state’s high-risk pool, in which the state assumes the financial risk but pays private insurers to administer coverage. Enrollees spend as much as one-third of their income on monthly premiums that cost as much as $796. Yet annual benefits are capped at $75,000.
Still, demand perennially outstrips the high-risk pool’s capacity, which has been reduced over the years as medical costs have risen and funding has remained largely limited to state tobacco tax revenue and enrollee premiums. Of 32 states with medical high-risk insurance pools, California’s is one of the largest, covering 7,800 people.
“The best estimate is it’s only serving about 10% of the people who are medically uninsurable,” said Beth Capell, an advocate with the consumer group Health Access California.
Most people in the high-risk pool have been rejected by at least one private insurer. Yet many turn out to be a bargain, paying more in premiums than they cost in medical expenses. In fact, 19% of the enrollees submitted no medical claims at all in 2004, the last year figures were available, and about 80% submitted claims for less than the average annual premium.
Good health, poor risk
High-risk enrollees include people like Scott Svonkin, who makes time for at least one tennis match each week. On a Burbank court after more than an hour of play one recent evening, he scrambled for a ball so far out of reach that most people wouldn’t have bothered. After the game, Svonkin’s fair skin was ruddy and sweat dripped from his forehead, but he was not out of breath.
After suffering from debilitating bouts of asthma as a child, he clearly relishes the ability he now has to exercise. He credits medications that weren’t around when he was growing up. But the very drugs that have allowed him to breathe freely for years may also have cost him his health coverage.
When Svonkin left his job, he picked up the premiums on the Blue Shield HMO his former employer had offered and extended his coverage for three years. That’s the maximum allowed under a federal law known as COBRA and a matching state law, both designed to make health insurance portable. A couple of months before that coverage was to expire, he asked Blue Shield to sell him an individual plan just like the one he was on.
But Blue Shield declined to sell him anything like that HMO plan, which included prescription benefits, he said. Instead, the carrier offered him a plan that did not cover medication.
Blue Shield declined to discuss Svonkin’s case, citing patient privacy laws, as did the other insurers that subsequently rejected him, Blue Cross and PacifiCare. Although the rejection notices pointed to various problems -- “expectant fatherhood” and swelling from a spider bite -- all three blamed his history of asthma, a condition that affects more than 4.5 million Californians.
Svonkin was able to enroll his wife, daughter and baby son in a private plan. But with nowhere else to turn, he reluctantly enrolled himself in the state’s high-risk pool. In an ironic twist, the pool assigned him to a plan administered by Blue Shield. His premiums are $479 a month -- far more than he figures he has cost the plan. The only medical expenses he has submitted in his first year on the plan have been his prescriptions, which retail for about $100 a month.
Blue Shield “wouldn’t take me at their risk, but they took me at the state’s risk,” he said. “The reasons they won’t sell me insurance are ludicrous because they can still make a profit providing me with healthcare.”
The ordeal has been an object lesson for Svonkin, who is now chairman of the county commission on insurance, an advisory panel to the Board of Supervisors. He uses his post to focus on the problems of the uninsured as well as the uninsurables. The county does not regulate insurers, but its clinics, hospitals and emergency rooms are overflowing with uninsured residents who have nowhere else to turn.
“Insurance companies are offloading sick people onto the county system,” Svonkin said. “They want a guarantee that they are going to make money. That’s why they won’t take sick people. They are missing the whole point about assuming some risk.”
*
(BEGIN TEXT OF INFOBOX)
These ills may be too risky to insurers
Health insurers in California have been allowed to keep secret their underwriting guidelines that determine who gets individual coverage and at what premium.
But a law that took effect Sept. 1 required them to report their underwriting guidelines to the Department of Insurance and the Department of Managed Health Care. It also required regulators to post the guidelines on the Internet, but without identifying which rules are used by which company.
Health plans also reveal a portion of their underwriting guidelines in letters notifying applicants why they were rejected, as well as in communications with brokers who sell their coverage.
According to regulators’ postings, rejection letters and interviews with brokers, conditions that can lead to outright rejection or a higher premium include:
AIDS, allergies, arthritis, asthma, attention deficit disorder, autism, bed-wetting, breast implants, cancer, cerebral palsy, chronic bronchitis, chronic fatigue syndrome, chronic sinusitis, cirrhosis, cystitis, diabetes, ear infections, epilepsy, gender reassignment, heart disease and hemochromatosis (a common genetic disorder that causes the body to absorb too much iron).
Other conditions are hepatitis, herpes, high blood pressure, impotence, infertility, irritable bowel syndrome, joint sprain, kidney infections, lupus, mild depression, muscular dystrophy, migraines, miscarriage, pregnancy, “expectant fatherhood,” planned adoption, psoriasis, recurrent tonsillitis, renal failure, ringworm, severe mental disorders, sleep apnea, stroke, ulcers and varicose veins.
-- Lisa Girion