South Africa’s coronavirus strain upends country’s vaccination plans

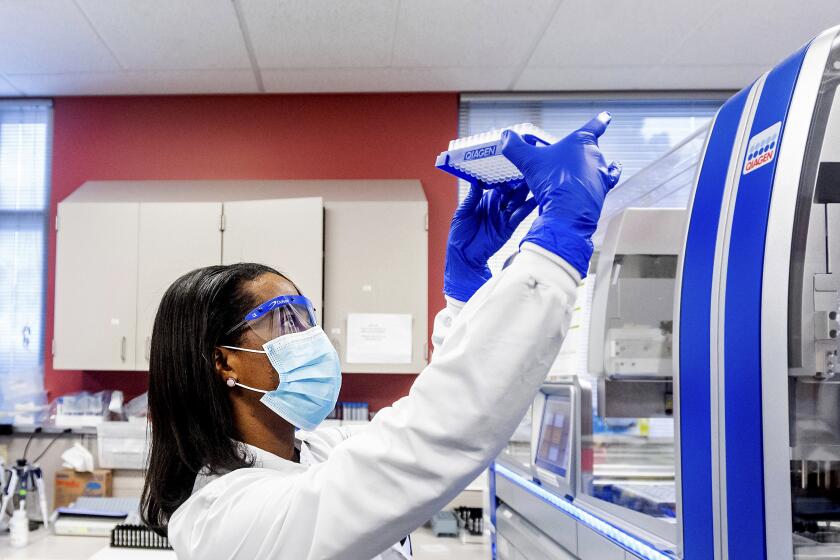
The coronavirus strain fueling a resurgence of COVID-19 in South Africa was not slowed down by a vaccine that officials had been counting on to protect its front-line healthcare workers, prompting the government to shelve plans for an inoculation campaign that would have begun this month.
“We have decided to put a temporary hold on the rollout of the vaccine,” Dr. Zweli Mkhize, South Africa’s health minister, said Sunday. “More work needs to be done.”
The experimental vaccine, developed by AstraZeneca and Oxford University, seemed promising just a few months ago. In clinical trials conducted in South Africa, people who received the vaccine were 75% less likely to develop mild to moderate cases of COVID-19 than were people who received a placebo. The government ordered 1 million doses.
“The AstraZeneca vaccine was showing tremendous potential,” said Dr. Shabir Madhi, a vaccine expert at the University of the Witwatersrand in Johannesburg.
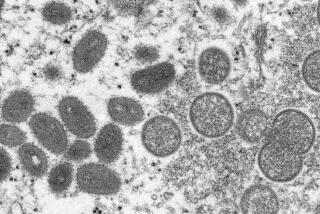
But that was before the emergence of a coronavirus strain called B.1.351, which is now dominant in South Africa and has spread to more than 30 other countries, including the United States. Since November, clinical trial participants who received the vaccine have fared no better than their counterparts who got the placebo.
Researchers once believed t would take months or even years for the virus to develop resistance to vaccines. The speedy evolution is largely a result of the virus’ unchecked spread.
Madhi and other scientists suspect this is because mutations in the virus’ genome have changed the shape of its spike protein, which is the vaccine’s primary target. That means the antibodies generated by the immune system in response to the vaccine are less well-equipped to neutralize the new version of the virus.
That problem isn’t limited to the AstraZeneca vaccine.
A COVID-19 vaccine developed by Johnson & Johnson reduced the risk of moderate to severe illness by 72% in clinical trial participants in the U.S. But in South Africa, the same vaccine reduced that risk by just 57% — and nearly all those who became sick were infected with the B.1.351 strain.
Similarly, a COVID-19 vaccine developed by the U.S. company Novavax was nearly 90% effective against all types of COVID-19 when tested in Britain, yet only 49% effective in South Africa.
“All of the vaccines that have currently been developed have been designed based on the original virus that was circulating,” Madhi said.
Madhi pointed to other concerning data from the trials of the Novavax vaccine: Some of the South Africans who got the placebo had already weathered a bout of COVID-19. In theory, their past coronavirus infections should have offered them some protection against the new strain. However, they were just as likely to be sickened by B.1.351 as people in the placebo group who had never had COVID-19.
COVID-19 patients who take months to overcome their coronavirus infections despite treatment can become incubators of dangerous new strains.
The AstraZeneca study that prompted Mkhize’s announcement involved a comparatively small group of about 2,000 people who were relatively young and healthy. A total of 42 of them developed COVID-19 during the course of the trial, including 19 who got the vaccine and 23 who got the placebo. From a statistical point of view, those who got the vaccine fared no better than those who didn’t.
“We have not proven that this particular vaccine protects against COVID-19,” Madhi said.
But that doesn’t mean it’s worthless.
Two-thirds of the study volunteers who became ill had mild cases of COVID-19, and the rest experienced moderate illness.
“What these data don’t tell us is whether or not this vaccine might still protect at least against severe COVID-19, especially in individuals that are at high risk of developing severe disease,” Madhi said. “That might still be biologically plausible.”
Mkhize agreed that the AstraZeneca vaccine might still be able to protect people from the worst effects of COVID-19.
“We’re uncertain about the impact of the vaccine, that it will have on hospitalization, severe diseases and death,” he said.
Tulio de Oliveira, an infectious-disease researcher at South Africa’s University of KwaZulu-Natal, noted that that the findings of the small trial are preliminary.
But even at this stage, the potential for new variants like B.1.351 to erode the effectiveness of vaccines underscores the importance of “coming up with next-generation vaccines,” he said.
Such vaccines might withstand the corrosive effects of new mutations by targeting sites on the virus that, unlike the spike protein, are less prone to change.
“We’re beginning to know where a virus can mutate and where it can’t,” said Dr. Bruce Walker, an immunologist and director of the Ragon Institute in Boston.
The Biden administration is boosting efforts to identify and track coronavirus variants to help scientists see where the pandemic is heading next.
Other efforts to overcome new mutations would recruit an entirely separate part of the immune system — its B-cells and T-cells — to recognize and kill the coronavirus. (A COVID-19 vaccine being developed by El Segundo-based ImmunityBio, headed by Times owner Dr. Patrick Soon-Shiong, aims to activate T-cells.)
In a study published Friday in the journal Science Advances, a group of cancer researchers working in mice was able to accomplish this by adding a so-called adjuvant — an ingredient intended to induce a stronger immune response — to their vaccine. The boosted vaccine recruited T-cells that provided strong protection to coronavirus-infected lungs.
“A vaccine like ours would have an independent set of weaponry to attack the virus by other means,” said co-author Dr. Christopher Haqq, head of research and development at Elicio Therapeutics. By prompting a T-cell response as well as antibody response, “we’d have a lot more shots on goal,” he said.
At the same time, the inevitable arrival of new coronavirus variants has prompted some researchers to acknowledge that not all COVID-19 disease needs to be prevented to bring the pandemic under control.
“Don’t look at overall efficacy,” said Dr. James Campbell, an infectious disease specialist at the University of Maryland School of Medicine. “Look at the efficacy for severe disease.”
Madhi agreed that preventing hospitalizations and deaths was the most important thing to focus on. A vaccine that can do that will still be valuable, he said: “I’ve become a little more realistic about what to expect from vaccines.”