UCI case report suggests antihistamines may provide relief for long COVID sufferers
- Share via
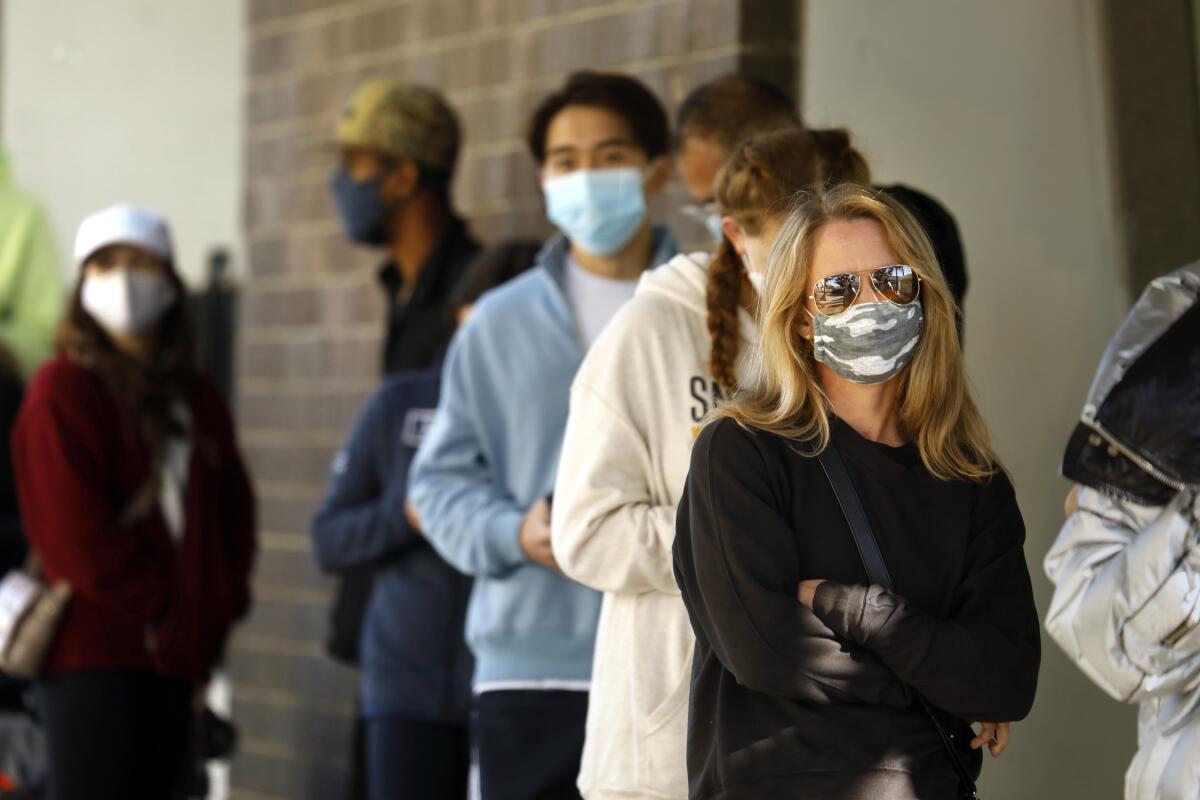
Shelves stocking over-the-counter cold and flu medicine stood almost barren at local pharmacies during the worst days of the Omicron-fueled winter surge.
But for sufferers of what’s commonly known as long COVID, could the allergy medication aisle offer relief of symptoms that persist after testing negative?
A new case report co-authored by UC Irvine nursing scholars and published in The Journal for Nurse Practitioners raises the question.
Referred to by doctors as post-acute sequelae of SARS-CoV-2, long COVID is “new” and “ill-defined” as described in the case report. The condition can encompass more than 200 reported symptoms and effect multiple organ systems.
It’s also widespread.
The case report notes long COVID as an “emerging health crisis.” As of August 2021, 54 million people suffered from the condition that can be disabling and for which there is no known cure.
Two healthy middle-aged women who suffered from long COVID but noted considerable improvement after taking antihistamines became the focus of the case report.
Melissa Pinto, a corresponding author and a UC Irvine associate professor of nursing, deems the recently published work as a “zoom in” on the bigger picture of long COVID.
It began with weekly meetings between a likeminded but nontraditional group of researchers and scholars.
Dr. Natalie Lambert, a case report co-author from the Indiana School of Medicine, scoured social media for health narrative data. The two cases in question were identified from Survivor Corps, a Facebook group that connects people who’ve suffered from COVID-19 with medical, scientific and academic researchers.
“This is the experience of two people,” Pinto said. “It gives an idea of when they took antihistamines, how long it took them to have relief, what type of combinations they used and what were the dosing regiments.”
In the first case, a relatively healthy white woman in her 40s contracted COVID-19 in January 2020. For almost a month, she suffered from an array of symptoms, including a dry cough, fever, rashes and fatigue.
By March, cognitive impairment, commonly known as “brain fog” and general fatigue, persisted. Long COVID affected her at work in the healthcare sector; she also couldn’t exercise as frequently or as vigorously as before infection.
Six months out, the patient stumbled upon something that finally gave her relief.
She took Benadryl after eating cheese, which triggered a dairy allergy, and noticed considerable improvement in both brain fog and fatigue the morning after. Long COVID symptoms returned when she didn’t take Benadryl for three days but once she did, her symptoms improved again.
Under the care of a doctor, she was prescribed a second antihistamine and reported a 90% return of her pre-COVID daily life and fully returned to work.
“We suspect that long COVID may have subtypes and this particular subtype, it may actually target these types of symptoms,” Pinto said.
In the second closely examined case, another healthy, middle-aged white woman reported long COVID symptoms nine months after infection, including brain fog, fatigue and a condition known as “COVID-19 toes.” More than a year after she was infected with COVID-19, she took an antihistamine and, like the first patient, experienced a marked improvement of her brain fog and fatigue the morning after.
Two months after a set dosage under a doctor’s care, she is reporting a 95% return to pre-COVID functioning and has been able to resume exercising.
Those findings are consistent with previous studies published in the Journal of Investigative Medicine as well as Pulmonary Pharmacology & Therapeutics, which both found potential benefits from treating long COVID symptoms with antihistamines.
“Right now, we have millions who are sick,” Pinto said. “Some can’t work, some are bed-bound. While we’re working on these larger questions surrounding long COVID, we need to help people get back on their feet.”
Antihistamines aren’t approved by the FDA to treat long COVID. Clinical trials haven’t been conducted to establish the efficacy of such medication and at what dosage levels.
Even still, with antihistamines being generally safe with few side effects and widely available, Pinto encourages long COVID sufferers to take the case report to their primary care physicians before treating symptoms with over-the-counter medication by themselves.
“I’m not instructing patients in any way to use this report as a guide to dose or anything like that,” she said. “I actually encourage patients, if they’re going to try antihistamines, to work with their provider.”
All the latest on Orange County from Orange County.
Get our free TimesOC newsletter.
You may occasionally receive promotional content from the Daily Pilot.






