Column: More signs that ‘gaming’ by the sick is not a problem in Obamacare
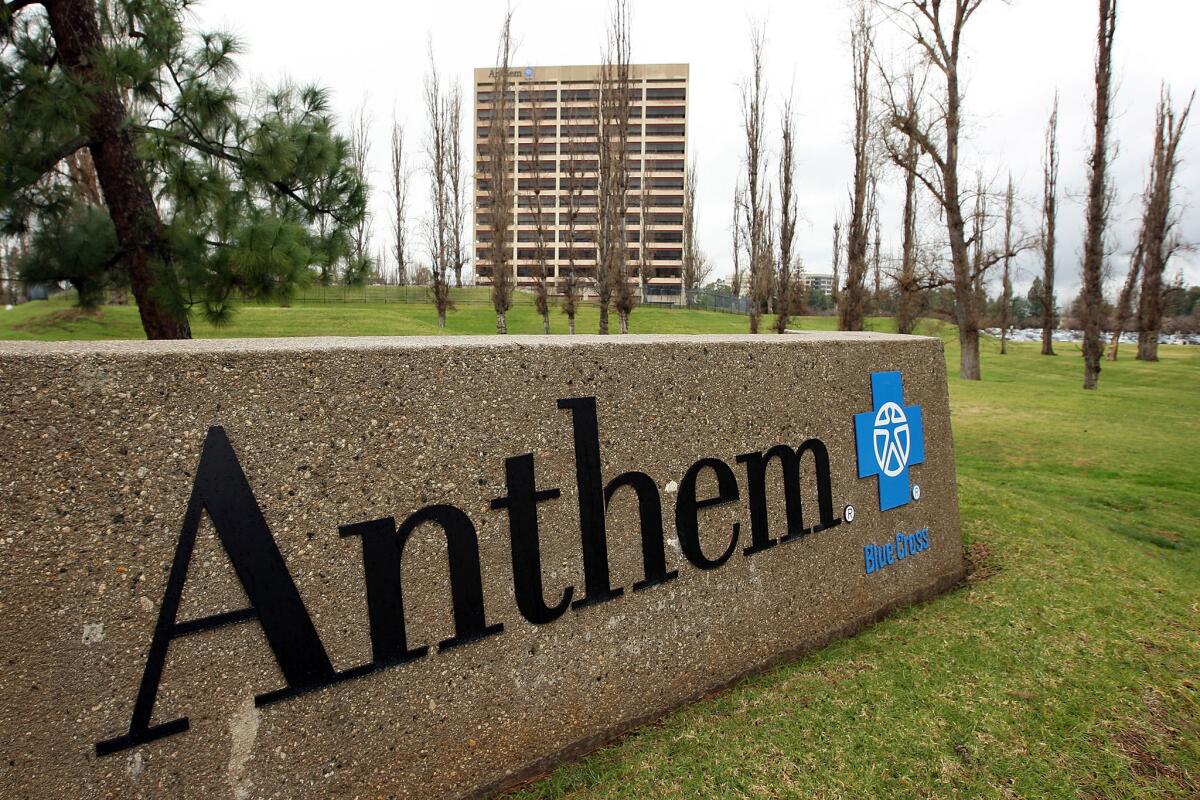
Giant insurer Anthem is among the companies claiming that insurance consumers are “gaming” Obamacare care, at its expense.
The one common element in assertions that thousands of Americans are “gaming” Obamacare by not signing up for health insurance until they get sick, thereby sticking beleaguered insurance companies with a big bill, is that none of these assertions come attached to any hard numbers.
Late last year, the Department of Health and Human Services invited insurers to produce the numbers, if they had them. It did so by proposing to tighten up on the so-called special enrollment periods, or SEPs, that allowed individuals to enroll in health plans outside the once-a-year open-enrollment window, and asking insurers to submit comments and data on the proposal.
We haven’t seen any comments laying out systematic abuse.
— Laurel Lucia, healthcare program manager at UC Berkeley’s Center for Labor Research and Education
Most big insurers submitted comments, as did AHIP, the health insurance industry’s trade group. None that I reviewed offered any empirical data -- just blanket assertions that people are gaming the system.
This has become an article of faith and a core complaint among insurers. The indispensable Charles Gaba of ACASignups.net posted a good update on the controversy on Tuesday. My skeptical take on the complaints appeared in December.
Since then, nothing has emerged to give substance to the insurers’ complaints. “We haven’t seen any comments laying out systematic abuse,” said Laurel Lucia, healthcare program manager at UC Berkeley’s Center for Labor Research and Education.
Instead, she argues in a recent article on the blog Health Affairs, the evidence points in the opposite direction -- that the majority of individuals eligible for SEPs aren’t taking advantage of them. Many of them are relatively young and healthy, so the result is that a disproportionate number of SEP enrollees are sicker than the general population. That’s exactly the trend that insurers should want to avoid.
The indications are that the insurers are wrongly treating SEPs as their enemy, when they should be trying to make them work better.
Indeed, some of the comments filed with HHS about SEPs seemed to be flagrant exaggerations of the problem. Aetna, for example, argued that slack enforcement of SEPs “poses significant threats [sic] to the viability of the risk pool.” The company counted “40+ SEPs for on-exchange coverage,” which “leave individuals with little incentive to enroll in coverage during open enrollment, since they can wait until they are sick ... and drop coverage immediately after receiving services.”
Is this plausible? To begin with, it’s hard to see how Aetna came up with more than 40 SEPs, unless it’s slicing them very thin. Aetna didn’t list them, and my generous examination of those listed by the government, treating every minor variation as a separate SEP, still came up in the mid-20s. (Is “gain or become a dependent due to to a child support or other court order” one SEP? Two? Four?)
The truth is that the SEPs fall into a handful of well-understood categories. These include “life events” such as getting married or divorced; becoming or gaining a dependent via birth, adoption or placement in foster care; or losing a job and the coverage that came with it. The qualifying events unique to the Affordable Care Act or other government assistance programs include becoming a U.S. citizen, moving to a new state or sometimes within a state, or experiencing a change of income that makes one newly eligible or ineligible for government subsidies. The government also allows special enrollments if a conventional enrollment was screwed up through no fault of the enrollee.
Some of these categories are expansive, but not all of them are entirely under the consumer’s control, and for Aetna to argue that they cover so many people that it leaves “little incentive to enroll in coverage during open enrollment” is simply preposterous.
Aetna must think the entire country consists of people plotting how to get a quickie marriage or divorce or have a baby just in case they get sick. The vast majority of SEPs cover a relatively trivial number of cases, unless you think there are hordes of people applying to become members of a Native American tribe after they get sick.
The insurers typically assert that an inordinately high percentage of new customers are coming in through special enrollment periods -- as many as 20%, by some reckonings -- and that those customers are unusually heavy users of medical services, especially in the first months after enrollment. That indicates “‘buying to use’ behavior,” the giant insurer Anthem said in its statement to HHS.
But that’s far from clear, Lucia said. She noted that the individual insurance market always has been subject to short enrollments and heavy “churn”; a study by the Kaiser Family Foundation in 2014 found that of people covered by individual policies in January 2010, only 62% still had that coverage by July and fewer than half were still on it after two years. The reason is that many people used it just as a bridge to employer-sponsored insurance or a government program such as Medicare. That’s still the case.
As for the mob undeservedly exploiting SEPs, there’s extensive evidence that the opposite is true. A study by the Urban Institute last year estimated that as many as 85% of people who were eligible to use SEPs to obtain insurance or fill coverage gaps failed to do so. Similarly, a study published last year by the University of Minnesota found a similar failure of outreach: “A large number of people are potentially eligible for special enrollment periods, and the majority of them are uninsured.”
Those researchers, like Lucia and HHS officials, have found that millions of SEP-eligible consumers remain unaware of their eligibility despite efforts by government agencies to find and educate them.
That leaves only the most motivated consumers to take advantage of SEPs -- those with medical needs. That doesn’t mean they’re deliberately gaming the system, only that they’re inclined to investigate their options. Ironically, tightening up the SEPs by shortening the windows of eligibility or requiring more documentation from those experiencing life events is likely to exacerbate the prevalence of sicker consumers in the SEP group. Forcing younger or healthy consumers to jump through more hoops before gaining coverage will prompt them to give up earlier than sicker patients.
The answer, Lucia said, is to make special enrollment more accessible to eligible people, not to find ways to turn them away. In California, for example, she proposed that the state insurance exchange, Covered California, coordinate with the state Employment Development Department “to connect individuals receiving unemployment insurance with health insurance.” The Department of Motor Vehicles could notify Covered California when people change their addresses.
What may be most important is to treat assertions of widespread gaming with a jaundiced eye. Insurance companies like nothing better than to simplify their business by eliminating uncertainties, including special enrollments. The fact that they all claim to see gaming happening, but can’t or won’t cite statistics or produce documents to prove it, should make everyone suspicious -- of them.
Keep up to date with Michael Hiltzik. Follow @hiltzikm on Twitter, see our Facebook page, or email michael.hiltzik@latimes.com
ALSO
How a huge insurance company screwed up on Obamacare
Dirty little secret: Insurers actually are making a mint from Obamacare
Ted Cruz flubs his family’s health insurance and (naturally) blames Obamacare