This $7,800-a-month cancer drug caused rashes and rarely worked. Now Trump could make FDA approvals even easier
In June, pharmaceutical giant Genentech sent doctors a letter saying they should no longer prescribe a blockbuster drug called Tarceva to most patients suffering from
A study had found that only a small number of patients — those with a certain gene mutation — might be helped by the drug, the company said.
The news upended a 2010 decision by the Food and Drug Administration to greatly expand use of the $94,000-a-year drug, despite warnings from a panel of experts that said there was little evidence it actually worked.
The FDA’s decision resulted in more harm than the hundreds of millions of dollars wasted on a drug that was ineffective for 90% or more of patients.
Over the years, thousands of patients were prescribed a drug that had no chance of helping them but could frequently cause terrible rashes covering their faces and bodies, according to prescription data and adverse event reports. Some patients with the most aggressively growing cancers died before trying other treatments that may have lengthened their lives.
The story of Tarceva shows the danger of approving experimental medicines before reliable scientific data show they are effective — which regulators are now doing more frequently.
Pressured by powerful pharmaceutical company lobbyists and often dramatic testimony by patient groups looking for hope, Congress has repeatedly loosened regulations to speed medicines to sale.
Some doctors fear the bar for approval will be lowered even more.
The FDA is now examining how to comply with the 21st Century Cures Act, a law Congress passed in December to hasten the approval of drugs and medical devices.
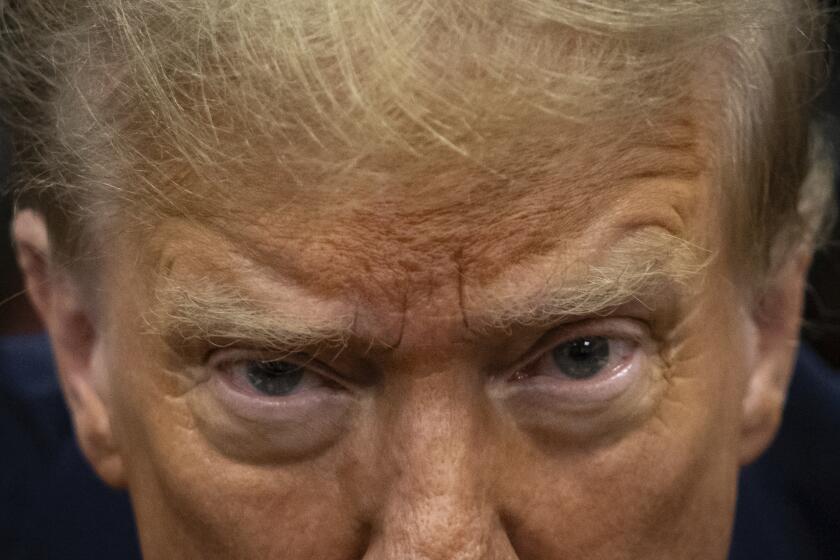
And critics of the FDA who say the review process still moves too slowly — including drug companies, their investors and patients desperate for new medicines — hope that President Trump will go even further. At a White House meeting with pharmaceutical executives this week, Trump promised them he was “going to streamline” FDA regulations.
“Every medicine puts you at risk of side effects,” said Vinay Prasad, a hematologist-oncologist at Oregon Health and Science University who has studied the FDA’s accelerated approval of cancer drugs. “The question is: Are those side effects worth it? For many of these drugs, we just don’t know.”
An FDA approval doesn’t necessarily mean that a drug works.
— Brian Shields, ex-Genentech sales rep and whistleblower
In a written statement, the FDA defended its fast approval of Tarceva and other medicines. The agency said lung cancer patients had few options when the drug was first approved in 2004.
The FDA said it had limited the drug’s approval to the small number of patients who had the mutation soon after Genentech released the results of the study last year showing it did not work for other patients. The agency had requested that study six years earlier.
How thousands of cancer patients were prescribed a drug that couldn’t help them
The Food and Drug Administration frequently speeds experimental medicines to sale by approving them before scientific evidence shows they work.
For a drug called Tarceva, the FDA’s decisions resulted in thousands of lung cancer patients taking a drug that could not help them.
Twelve years passed before the agency warned doctors in October that Tarceva only worked for a small number of patients with a rare gene mutation.
FDA officials attributed the delay in limiting Tarceva’s approval to the many years it can take to perform a meaningful scientific study.
“This process of gaining new knowledge about disease and drug efficacy — which can significantly modify or even contradict results on which previous drug approval decisions were made — is the essence of scientific advancement,” the agency said.
Genentech declined to make executives available for interviews. The company and its marketing partner OSI Pharmaceuticals instead sent a brief statement.
“Clinical trials answer specific questions about the safety and efficacy of a medicine, but also lead to new hypothesis-generating information,” the statement said. “It is not uncommon for a medicine’s approved indications to change over time.”
One of Trump’s possible selections to head the FDA — Jim O’Neill, a Silicon Valley venture capitalist with no education in medicine or science — has raised the idea of approving drugs with no tests of their effectiveness.
“Let’s prove efficacy after they’ve been legalized,” O’Neill said in an August 2014 speech at a biotech conference.
That would mean more patients would become part of a continuing experiment and be prescribed medicines their doctors know little about.
Tarceva is not the only medicine that doctors are now prescribing that may not work for most patients. In a study, Prasad and his colleague found that of 36 cancer drugs approved by the FDA between 2008 and 2012, only five had been shown to actually extend survival by 2015.
Some ineffective drugs have eventually been taken off the market, but it can take years. A drug called Mylotarg was pulled from pharmacy shelves in 2010 — 10 years after the FDA approved it for acute myeloid leukemia, a bone marrow cancer.
Scientists designed Tarceva to block an enzyme associated with epidermal growth factor receptor, or EGFR, a protein believed to play a role in the formation and growth of cancer.
In 2004, researchers discovered a gene mutation tied to EGFR, creating a way to find those patients more likely to respond to the drug.
Many patients with the mutation have lived for months or even years while taking Tarceva.
Yet for years, Genentech and OSI downplayed the importance of testing for the mutation or levels of the protein and avoided using those tests to narrow the pool of patients. Instead the companies’ early trials — and promotion of the drug — were aimed at all patients with non-small cell lung cancer whether they had the mutation or not.
Former Genentech scientist Paul Waring explained more about the executives’ decisions in a presentation at the Walter and Eliza Hall Institute in Australia in 2014.
He told the crowd of scientists that in 2006 Genentech’s commercial team had estimated the company would lose $150 million a year in Tarceva sales if in its next trial — which it was planning to look at early-stage lung cancer — it stopped accepting all patients and instead restricted enrollment to those testing positive for the protein.
“We struggled — boy, did we struggle — with this decision,” Waring told the crowd. “The company was obviously keen to protect its revenue base.”
Yet by keeping all patients in the trials, even though other researchers had shown 10% or less might respond to the drug, the corporate scientists were having a hard time showing Tarceva offered an advantage over the placebo.
Instead, in the trials, the few patients who improved dramatically boosted the survival results for the overall pool of volunteers taking the drug. At the trials’ end, the group taking the drug looked just slightly better than those taking the sugar pill.
In essence, each trial was a lottery. Only a small number of patients won even though the companies sold hundreds of tickets.
When Genentech and OSI went back to the FDA in 2009 and asked that Tarceva’s approval be expanded, their new trial showed the drug increased survival by a month.
The FDA had initially approved the drug in 2004 as a treatment for severely ill patients who had failed chemotherapy and had few other options. Now the companies wanted it to be prescribed as “a maintenance therapy” for patients who were not as ill and had responded to chemotherapy.
OSI Chief Executive Colin Goddard told investors in July 2009 that the expanded approval could add more than $500 million to Tarceva’s annual sales in the U.S., more than doubling them.
To bolster their case at a hearing on the proposal, the companies paid for several patients to fly to the FDA’s offices outside Washington, D.C., to testify about how Tarceva had saved their lives.
Two patient advocacy groups, which had received part of their budgets from Genentech and OSI, also pleaded for the expanded approval.
“My cancer is being controlled by this drug, which I am so thankful for,” said Mary Lou Fisher of Fortuna, Calif., in a statement read at the hearing.
The committee of experts advising the FDA was not swayed. They voted 12-1 against expanding Tarceva’s approval.
“I think there’s uncertainty, substantial uncertainty, about what the actual added benefit is,” said Thomas Fleming, a biostatistics professor at the
“We were presented with a single study … that has some design flaws showing some very modest or even minimal benefit,” added Ron Richardson, an oncologist at the Mayo Clinic who also voted against the approval. “I don’t think the sponsor answered the question on the value of this drug.”
The FDA did not take the experts’ advice.
The agency employee signing the 2010 approval letter was Robert Justice, a former Genentech senior scientist.
The approval further fueled Tarceva’s global sales to nearly $1.5 billion in 2011, according to QuintilesIMS, a consulting firm. American doctors wrote 119,047 prescriptions that year.
In sales brochures, Genentech and OSI touted Tarceva for having “a proven survival benefit” and working “in a broad patient population.” One flier showed an older man reading to a young boy. “For moments that matter,” the tagline said.
Brian Shields, a former Genentech sales rep, said he complained in a 2010 meeting of the Tarceva marketing team that the company was promoting the drug to patients it could not help. His boss dismissed his concerns, he said, telling him he “was not a team player.”
Shields later filed a lawsuit as a whistle-blower under the federal False Claims Act, which the government joined. The suit claimed Genentech and OSI had illegally sold the drug, including by sending doctors and nurses to attend all-expense-paid retreats at resorts where they were “groomed” to tell others about how Tarceva could extend survival in “a broad range of patients.”
The companies also recruited patients whose cancers had responded to the drug, and then trained and paid them to talk to others in what it called the “Patient Ambassador Program,” his lawsuit said.
The companies discouraged doctors from testing patients for the mutation, the lawsuit said, because they knew it would reduce sales.
“This is a failure of the system,” Shields said in an interview. “An FDA approval doesn’t necessarily mean that a drug works.”
On June 6, 2016, the
For bringing the case to authorities’ attention, Shields received about $10 million of that amount.
As you lower the regulatory standards you open the flood gates to more of these ineffective drugs.
— Vinay Prasad, Oregon Health and Science University
Three weeks later, the companies sent physicians an “Important Correction of Drug Information.” They warned doctors to stop prescribing the drug except to the minority of patients with the mutation. The letter revealed the results of the study the FDA had requested six years earlier. It showed that patients without the mutation died at the same rate whether they got Tarceva or the placebo.
Genentech and Astellas said they believe their promotional practices were “entirely proper and in compliance with the law.” They said they settled the lawsuit only to avoid more costly litigation.
“It takes years to design clinical trials, recruit patients and evaluate results,” the companies said in a statement. “As we learned more about disease biology, we worked with the FDA to design a study that looked at Tarceva in people with EGFR mutations.”
Waring, the former Genentech scientist, said in an interview that he believed the company had moved as quickly as it could in determining the drug only worked for those with the mutation.
“We were all on a steep learning curve,” he said.
But Prasad, the Oregon Health and Science professor, said the FDA’s lax approval standards, combined with the six-figure prices companies can charge for unproven or marginal medicines, have encouraged the industry to take marketing shortcuts rather than spend research dollars to find true breakthroughs.
Prasad pointed to a study that found the average gain in survival for the 71 cancer drugs approved from 2002 to 2014 was just 2.1 months.
“That’s not good enough for the people I see in my clinic,” he said. “As you lower the regulatory standards you open the flood gates to more of these ineffective drugs.”
Follow @melodypetersen on Twitter
ALSO
Pelosi calls Trump's plan to dismantle financial regulations a 'massive con' and vows to fight it
Apple, Facebook, Google and other tech giants join fight against Trump's travel ban