A bitter pill for Big Pharma
The strategy that has made the pharmaceutical industry one of the wealthiest and most powerful on Earth is finally starting to betray it.
Beginning in just a few weeks, and continuing over the next several years, some of the biggest-selling and most profitable drugs in history will lose their patent protection. When the 20-year patent on a drug expires, its sales plummet because other companies can sell generic versions for a fraction of the price.
Merck, for instance, will lose its patent on Fosamax, the top-selling osteoporosis medicine, on Feb. 6 -- and can expect to see a swift decline in its $3 billion in annual sales. Then, later this year, Johnson & Johnson is expected to lose its monopoly on Risperdal, the $4-billion-a-year antipsychotic drug. The greatest loss of all will be suffered by Pfizer, the maker of Lipitor, the bestselling drug in the world. The $12-billion cholesterol-lowering pill is expected to go generic as early as 2010.
Of course, it was no secret that these patents would expire. Everyone in the industry knew that time would run out on these monopolies. The real problem is that the industry’s scientists have hit a dry spell. They are not discovering enough new drugs to replace the aging standbys. Last year, the U.S. Food and Drug Administration approved just 19 new medicines, according to preliminary data, the fewest since 1983.
Moody’s, the bond-rating company, sounded the warning on Wall Street last fall. The firm said the financial outlook for the wildly profitable pharmaceutical industry had turned sour. Some companies, the firm said, faced the loss of as much as half their revenues. The Wall Street Journal followed up on the report last month with a front-page story headlined “Big Pharma Faces Grim Prognosis.”
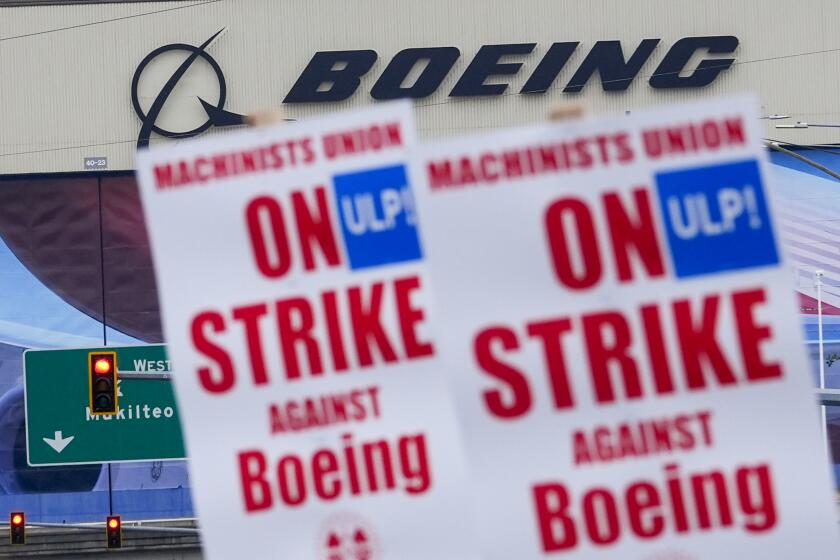
Lost in all the hand-wringing on Wall Street is a recognition of how the industry got itself into this fix in the first place. For 25 years, the drug industry has imitated the basic business model of Hollywood. Pharmaceutical executives, like movie moguls, have focused on creating blockbusters. They introduce products that they hope will appeal to the masses, and then they promote them like mad. The strategy has created not only Fosamax and Lipitor but Prozac for depression, Nexium for heartburn and Viagra for sex.
Only now is it becoming clear that this business model couldn’t work forever. The strategy had a flaw that executives have long ignored: It required extraordinary amounts of promotion at the expense of scientific creativity. To make the strategy work, the drug industry put its marketers in charge; scientists were given a back seat. Is it any wonder that executives at many companies have watched their pipelines of new drugs slow to a trickle?
The story of the industry’s first blockbuster pill -- the heartburn drug Zantac -- helps illustrate why marketing has long ruled over science inside the big drug companies.
Introduced in 1983, Zantac was not actually a new drug. Glaxo, its maker, simply copied the innovative work done by scientists at a rival company. Those scientists had worked for years before discovering a drug so original that it changed the practice of medicine. Their invention, Tagamet, was the first pill to heal ulcers. Before its introduction, ulcer-plagued patients had few options other than a surgeon’s knife.
Rather than spending money on research to find its own breakthrough drug, Glaxo went after the easy money. Its scientists tweaked the chemical formula of Tagamet so that it was just different enough to secure its own patent. Glaxo then set the price of Zantac as much as 50% higher than Tagamet and poured the extra revenue into a marketing campaign so effective that executives still talk about it. Glaxo promoted Zantac not just for ulcers but for heartburn (or what the company preferred to call the more frightening “gastroesophageal reflux disease”). By 1988, Zantac was the industry’s bestselling drug.
This focus on copycat pills is not terribly different from what movie studios have been doing for decades -- seeking mega-profits by promoting the sequel to the sequel of the blockbuster released years before. Hollywood has long understood the magic of marketing. As the late movie producer Joseph E. Levine reportedly explained, “You can fool all the people all the time if the advertising is right and the budget is big enough.”
Drug executives say they must spend as much as $1 billion to promote a drug in its first two years on the market if they want it to become a “mega-brand” that will bring in sales of more than $1 billion a year. This extreme spending on promotion is why the chief executives of today’s drug companies are less likely to be scientists than they are to be marketing gurus, salesmen, lawyers or Harvard MBAs. AstraZeneca and Johnson & Johnson, for instance, are run by men who began their careers as pharmaceutical sales reps. Pfizer became the biggest drug company in the world under the watch of William C. Steere Jr., who started as a Pfizer salesman. Now, Pfizer is piloted by a lawyer who joined the company from McDonald’s.
Some big drug companies even moved marketers into their laboratories. Pfizer, for example, sent marketers to its labs in the 1990s in a program dubbed CRAM, or “Central Research Assists Marketing.” The name made it clear who was calling the shots. “We try to make sure that research is not developing something that no one particularly wants,” Dr. John F. Niblack, Pfizer’s top scientist, explained in 2000.
The pharmaceutical companies have become so clever at promotion that even drugs that work little better than a sugar pill have become mega-sellers. Just look at the heavily prescribed class of antidepressants that includes Zoloft and Paxil. Scientists have performed dozens of clinical trials to test these drugs, and in roughly half of them, the sugar tablet worked just as well or better than the drug. We know this because enterprising researchers recently tracked down data the companies decided years ago not to publish and described it in an article in the New England Journal of Medicine.
The medicines might not always work, but the business model worked miracles for the corporate bottom line. Between 1980 and 2003, the amount Americans spent yearly on prescription drugs rose from $12 billion to $197 billion, creating growth rarely seen in such an established business. While Americans doubled their spending on new autos between those years and tripled what they paid for clothing, they increased their spending on prescription drugs by nearly 17 times.
Patients have not been so lucky. A drug is not like a movie. Each one has potentially deadly risks. In fact, the industry’s blockbuster mentality has helped lead to thousands of needless deaths.
These tragedies have occurred because executives do everything in their power to get doctors to prescribe a newly approved drug to as many patients as possible. Wall Street watches a drug’s first few months of prescriptions just like it focuses on a movie’s opening weekend at the box office. A disappointing launch of a new pill can mean a plunge in the company’s share price and in the value of its executives’ stock options. So early sales are critical.
Even as companies relentlessly promote the new pills, doctors know little about them. A new drug may have been tested in only a few thousand patients before being approved by the FDA, but is swiftly prescribed to millions. Time and time again, new drugs have been found to harm patients in ways not apparent in their early trials.
This was heartbreakingly evident in the case of Vioxx, the heavily promoted pain reliever. It was prescribed to more than 20 million patients before Merck pulled it from the market in 2004 because it doubled the risk of heart attack. An FDA scientist estimated that Vioxx might have caused heart attacks or strokes in as many as 139,000 Americans and that 30% to 40% of them died.
At the same time, the blockbuster model has failed to produce drugs that the sick desperately need. For example, executives have shown less interest in medicines like antibiotics that actually cure disease than in those that only treat symptoms. Most blockbusters are pills for conditions such as anxiety, high cholesterol or constipation that must be taken daily, often for months or years. They are designed for rich Americans who can afford to buy them. Medicines for tropical diseases, including malaria, which is devastating the developing world and killing a child every 30 seconds, have never been an industry priority. The poor can’t pay the high prices that a blockbuster demands.
Even medicines for diseases afflicting Americans are not pursued if the number of sufferers is too small.
This became clear when Bristol-Myers Squibb executives announced at a news conference in 2000 that they were embarking on what they called the “MegaDouble” business plan. To enhance the company’s profits, executives ordered its scientists to work only on “mega-blockbusters,” such as Lipitor. Scientists with blueprints for drugs promising a mere $100 million in annual sales had little choice but to box up their work and send it to the warehouse. (And executives are now perplexed about why they don’t have enough new drugs.)
It would be wrong to believe that this is the end of the industry’s wealth and power. Some companies, including Pfizer and Bristol-Myers, are laying off thousands of employees. But these companies have been so profitable for so long that they are merely starting to shed bloated operations. For example, Pfizer executives explained when they began reducing the sales force that they would now have two sales reps call on each physician -- down from three or even more.
As some firms struggle, patients will bear the brunt. The prices of brand-name drugs will rise even faster. Promotional campaigns will become more aggressive. Marketers will reintroduce old drugs -- modified just enough to secure new patents -- and tell us they are new.
This month, Eli Lilly celebrated the approval of its latest drug: a remake of Cialis, its sex pill that was a copycat of Viagra. Faithful to the blockbuster model, the new Cialis is not just taken when needed for sex, but every day.
Melody Petersen covered the drug industry for the New York Times from 1999 to 2003, and is the author of “Our Daily Meds,” which will be published in March.
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.