As NECC is sued, meningitis outbreak’s patient zero is autopsied
With the toll from the fungal meningitis outbreak up to 21 dead and 247 sickened, and as the compounding facility responsible for fungus-tainted drugs is hit with a lawsuit, researchers have looked back at the first case that alerted them to the disease. Their results were published online Friday in the New England Journal of Medicine.
The epidural steroid injections were produced at the New England Compounding Center, which shut down production and recalled all its products Oct. 6. About 14,000 patients are believed to have received injections. (The company is now being sued by Peter McGrath, a former federal prosecutor, on behalf of an unnamed plaintiff in Boston, according to the Chicago Tribune.)
Patients receiving injections of preservative-free methylprednisolone into their spinal cords to treat lower back pain have been diagnosed with meningitis in 16 states, with Tennessee the hardest hit.
Now doctors at the Vanderbilt University School of Medicine in Nashville, Tenn., have reported their results from an autopsy of the first medically diagnosed patient felled by the outbreak — a 50-year-old man with a history of degenerative lumbar-disk and joint disease — and recounted the disease’s progress.
The patient first came in with a headache and neck pain that had worsened over eight days. Doctors noted that the meninges — the protective membrane encasing the brain and spinal cord — were showing signs of irritation. There was a spike in white blood cells, a typical sign the body was under attack. But tests for bacteria in his cerebrospinal fluid were negative, and he was discharged and prescribed drugs to fight meningitis (which is typically caused by bacteria or viruses.)
A week after being discharged, though, the patient was back with a worsening headache and back pain. His white cell count was now 4,422 per cubic millimeter (above 5 cells per cubic millimeter is considered abnormal).
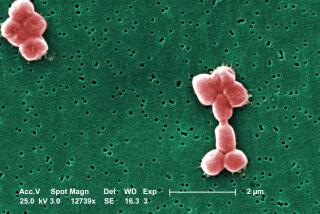
By Day 6 in the hospital, he was experiencing extreme drowsiness and subject to “intermittent staring spells.” The next day, the microbiology lab said they’d picked up signs of the fungus Aspergillus fumigatus in his body.
On Day 11, he suddenly became unresponsive and appeared to be experiencing seizures. By Day 15, the damage to his cerebrum and cerebellum was so extensive that there was little hope of neurologic recovery. Life support was discontinued, and he died on his 22nd day in the hospital.
Strangely, this patient was the only one diagnosed with a species of fungus called Aspergillus fumigatus – it hasn’t yet been detected in other cases, according to an accompanying commentary in the journal written by three doctors. Other cases have pointed to the fungus Exserohilum rostratum.
Early in the outbreak, according to the commentary, patients suffered their symptoms for weeks. Now they’re getting patients checked and treated when even very mild symptoms appear. That’s particularly important, since symptoms from fungal meningitis are typically more subtle than in bacterial meningitis, the authors point out. Later cases have since been milder — possibly because they’re being caught sooner.
“The hope is that early diagnosis and treatment will avert severe complications, such as strokes,” the authors write.
Here’s a recent Q&A; addressing questions raised by the outbreak. For updates, visit the CDC website.
Follow me on Twitter @aminawrite.