So much data-gathering, so little doctoring
I’m a stomach doc. I’ve seen thousands of patients, inside and out, for 25 years. I’ve done research, I’ve taught, I’ve been an administrator. And as the years rolled by, I’ve watched the healthcare industry begin to undo healthcare itself. It’s complex, cumbersome and bureaucratic, and the bigger the practice or the clinic or the hospital and research facilities — like the universities I used to work at — the worse the problem.
For a physician and his patient, the exam room visit is everything. Healing begins right then and there. The process of telling your story, being heard, being touched and feeling connected to your doctor is an incredibly powerful element of healing. While we’re bombarded with the latest and greatest discoveries and inventions of medical science, the fact of the matter is that most people who walk into a doctor’s office don’t have some horrible disease. They simply don’t feel well. My job is to listen and observe, to figure out who really does have something bad going on and who may simply be feeling the effects of life’s wear and tear.
There’s a huge difference between that and the healthcare industry, which is more about industry than health or care. Third-party payors don’t really care what happens in an exam room. The visit that you, as a patient, have been anxiously waiting for could just as easily be shoes or oranges or pork bellies to these folks. It’s just a commodity. It’s just data. And now the industry wants it documented in a format that works for billers and statisticians but not so much for doctors: the electronic medical record.
That’s the note your doctor is probably busy pecking away at while you’re trying to explain what ails you. In theory, an EMR should make care better and more efficient. It’s falling pretty far short of that goal.
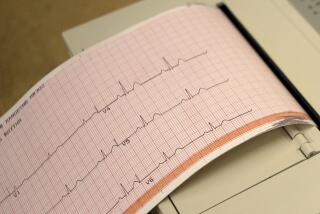
For starters, a lot of the software is clunky and the way it asks for information is unnatural. It can take more time to complete the “necessary” documentation for a colonoscopy or other endoscopic procedure than it took to do the procedure itself. Doctors and nurses and lab techs suddenly have to be data-entry clerks, filling in multiple “fields” and negotiating drop-down menus.
I’ve seen nurses get so busy typing what they do, they can’t do it. I’ve watched when an alarm sounded, indicating that a patient was breathing inadequately — the sensor had simply fallen off the patient’s finger. The nurse, back to the patient and typing furiously, shouts “Breathe!” without ever looking around. These aren’t bad nurses; they’re good nurses in bad situations.
I had my first encounter with an electronic medical record as a patient at my internist’s office. I consider him to be a model physician: smart, conversational, part friend and part counselor. I was pretty stunned, then, when I mostly saw he back of his head as he asked me questions and typed, badly.
“Hey, Jeff, does any of this look like a good doctor-patient interaction?” I asked.
“Hell, no,” was the prompt reply. “But I’ve got to do this now or I’ll never get finished on time.”
Whatever the EMR may become, right now it’s mostly a receipt for a transaction, a bill of sale. We all want to be sure we’re getting what we pay for. The government and insurance companies are no different — they require lots of documentation. What gets entered into the “elements of the encounter” field on the EMR determines how much the insurance company will pay, which only makes the unholy mess of electronic medical records worse.
With doctors everywhere working more for less, the pressure is on to perform lots of “elements” and to treat these notes like an old Chinese restaurant menu: “One from column A, two from column B …”
It used to be that a physician’s note contained dubious penmanship but concise, insightful information that guided the evaluation and treatment of the patient. Now notes are pages long, often containing verbiage simply cut and pasted from previous notes so as to speed the awful process or maybe to fulfill the requirements for “billing at a higher level.” I may have to dig through scads of detailed “data” that justify payment but don’t necessarily result in better care.
This system clearly needs some work. Or a boycott.
When I chose to leave the world of academic medicine for private practice, I went back in time. I joined a small practice that prides itself on service. There is no answering machine. Your call is answered by an honest-to-goodness human being. Because it’s a small group, we’re not yet required to switch to electronic medical records. I write, by hand, notes that contain the information I need to help you feel better. When I finish our visit, I dictate a letter and often call or text your referring physician to let them know what’s going on. I bill based on the notes, but no one’s costing out the “elements of the encounter.”
So old school. So unacceptable. So effective.
I feel as if I’ve stumbled into a medical oasis. My time is spent being a doc rather than a scribe or grocery clerk ringing up a sale. My time is spent interacting with a person who wants my help; it isn’t diluted with a perverse treasure hunt for clinically irrelevant but EMR-encouraged information. I’m happier in my work than I have been in a decade. My patients now are happier than my patients then. Everybody recognizes and responds to good service, whether it’s in a doctor’s office or an auto repair shop.
I have no doubt that my little oasis will come under the thumb of the new era of healthcare. And when that happens, we’ll do our best to make it work for our patients. But for now, while it lasts, I’m going to enjoy being the kind of doc that I always wanted to be.
Michael P. Jones is a gastroenterologist in Virginia.
Find additional essays in the Labor Pains series. Has your work changed in recent years? Tell us about it by email at laborpains@latimes.com or on Twitter at #latlaborpains.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.