U.S. seeks to speed up production of Ebola drug

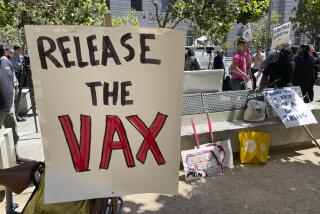
With the Ebola outbreak threatening to spiral out of control, U.S. officials unveiled a multimillion-dollar plan Tuesday aimed at getting a promising drug out of American research labs and into African hospitals and clinics more quickly.
The initiative comes not a moment too soon: After expediting a clinical trial with monkeys and supplying the drug to a small number of human patients, the firm that developed ZMapp has no more in its cupboard.
But even with nearly $25 million to speed the manufacture and testing of the experimental therapy, experts said, it probably won’t be ready in time to help the tens of thousands of people likely to be infected by the Ebola virus in the coming months.
In the worst case, it may turn out that the biologic therapy offers no help to those fighting the often-fatal hemorrhagic fever.
“We don’t know yet whether it works,” Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, said Tuesday after returning from a fact-finding mission in West Africa. “If it does, we don’t have it. So we can’t rely on it.”
Five patients who received the experimental drug are still alive, including two American aid workers who made full recoveries after being evacuated to the U.S. for treatment. Two other patients — a Liberian physician and a Spanish missionary priest — died despite taking ZMapp.
So far the outbreak has sickened at least 3,070 people and killed 1,552 in five countries, according to the World Health Organization.
A study published last week in the journal Nature raised hopes that the medication might be an elixir of deliverance. Among 21 macaque monkeys infected with Ebola, all 18 who got three doses of ZMapp — including some who were only days away from death — were able to clear the virus from their systems. The three animals that did not receive the drug died.
Those findings prompted the study authors to call for safety tests in humans “within the next few months” so that the drug could be delivered to patients “as soon as possible.” Yet for all the promise, the manufacturing process required to make ZMapp can take roughly half a year.
Indeed, there are a welter of logistical, regulatory and economic challenges to ZMapp’s large-scale production and use. Those challenges, experts said, prompted the Department of Health and Human Services to devote $24.9 million over 18 months to help San Diego-based Mapp Biopharmaceutical Inc. accelerate production. The funding could be increased to $42.3 million if deemed necessary.
The medication is a biologic therapy — it involves genetically engineered antibodies that mimic those of the human body. The molecules latch on to carefully targeted proteins on the Ebola virus and mark them for destruction by the host’s immune system.
Creating armies of cloned immune cells to turbocharge the body’s own defenses is a new approach to fighting disease. But it’s already the basis for dozens of drugs approved for use in the U.S., including the cancer drug Avastin and the rheumatoid arthritis drug Enbrel.
What’s different about ZMapp is the way cloned cells — called monoclonal antibodies — are made. Instead of being incubated in the cells of mice, rats or Chinese hamsters, the antibodies at the heart of ZMapp are grown in tobacco plants.
After scientists identify and design the specific cocktail of antibodies that will beckon the immune system’s defenses, they genetically engineer a plant virus to ferry them into the plants. (Plant viruses are not dangerous to people.) The infected plants are grown in windowless hydroponic warehouses under artificial lights. There’s no dirt, which might contain contaminants, just water and plastic mesh, and a conveyor system that ferries the plants around so they get the optimal amount of light.
The tobacco plants incubate both the virus and its cloned antibody cargo. But in seven to 10 days, the virus kills the plant, turning it yellow and causing it to wilt. The dying plants are harvested and ground into a green sludge. After the proteins in the mixture are distilled and purified, the result is a vial of colorless liquid.
To produce the 10 grams of antibodies needed for a single course of ZMapp, Mapp Biopharmaceutical currently requires 30 to 50 kilograms of tobacco leaves — the capacity of a small greenhouse. If tobacco plants could be engineered to produce antibodies more efficiently, that volume could be reduced to about 10 kilograms, said Charles Arntzen, an Arizona State University microbiologist who pioneered the process by which “plantibodies” are made.
Now that the key antibodies have been identified — a project Mapp Bio scientists worked on for years — it takes four to six months to produce a clinical-grade medicine. That’s a land speed record compared with the 12-to-20-month process used in making biologic drugs the conventional way, said Dr. Michael Kurilla, director of the Office of Biodefense Research Resources and Translational Research at the National Institute of Allergy and Infectious Diseases.
Another key roadblock is the novelty of the ZMapp production process. The Food and Drug Administration has yet to draft the quality-control strictures that would govern the large-scale production of plantibodies.
To date, the FDA has approved only one other biologic therapy that uses a similar process: In 2012, the Israeli firm Protalix Biotherapeutics won the agency’s blessing to sell a drug for Gaucher’s disease that is manufactured in carrot cells.
“I’m sure the FDA has tools to evaluate each technology on its own,” said David Aviezer, chief executive of Protalix. But the relative novelty of ZMapp’s production process adds “another step” that could create delays in getting ZMapp to the epidemic’s front lines, he said.
Under the new federal contract, Mapp Bio will make “a small amount of the drug” for use in human safety trials, according to the Department of Health and Human Services. Government officials, company scientists and independent experts will also explore ways to ramp up production and speed the development of regulations to ensure the drug can be made in large quantities.
Dr. Robin Robinson, director of the department’s Biomedical Advanced Research and Development Authority, said the first lot of ZMapp “is now under production.” That lot will be used in human trials scheduled to begin at the end of 2014 and to conduct additional animal studies of its safety and effectiveness, he said.
Ultimately, ZMapp could be made somewhere in Africa, and South African officials are in talks with U.S. officials and Mapp Bio to develop a production facility there, according to Ed Rybicki, director of the University of Cape Town’s Biopharming Research Unit.
“We most certainly have the expertise and the necessary infrastructure to support a facility,” Rybicki said. “Trouble is, it needs to be built.”
Twitter: @LATMelissaHealy