When insurers don’t pay for surgery
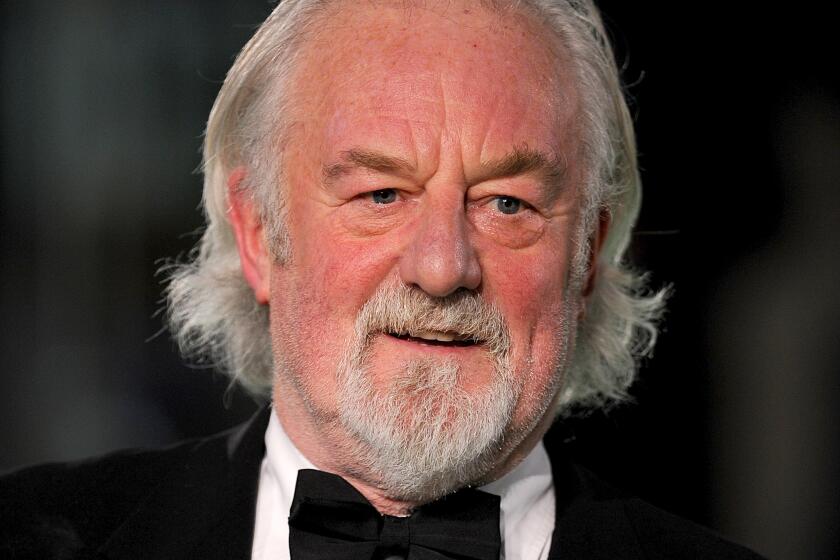
Peter Altschuler’s back surgery had been a long time coming. The 66-year-old marketing professional and actor from Santa Monica slipped a disc about 10 years ago, and he’s been coping with it ever since.
A series of injections kept him pain-free for years, he said, but by 2012 they stopped doing their job. “I was in constant discomfort,” he says. His doctors said it was time for surgery.
Although old enough to qualify for Medicare, Altschuler held on to an insurance policy he’d had through a professional association before turning 65.
As most health plans do, his insurer required him to obtain prior approval for his procedure. So he worked with his doctors to submit the required paperwork. It included the medical justification for his surgery, and he eventually got the green light.
But six weeks after his procedure, he got another notice, this time saying his plan wouldn’t cover the cost of the surgery after all. Now, instead of a $2,500 bill, he is being charged $100,000.
There are many reasons insurers deny payment for medical bills, even for procedures that were approved ahead of time. Here is a look at what can happen and what you can do about it.
Fighting over medical necessity. Insurers’ decisions about whether to pay for a procedure are based typically on whether it’s considered medically necessary, says Dr. Robert A. Bitonte.
For insurers, “if the determination is that it’s not medically necessary, they can decline it,” he says. Bitonte is a member of the Los Angeles County Bar Assn. and past president of the Los Angeles County Medical Assn.
Insurers review cases both before and after a procedure, and they can come to a different conclusion based on what took place in the operating room.
“Medically necessary care has to be provided. The law is clear on that,” Bitonte says. But how the determination of what’s medically necessary is made and who has the primary right to decide — doctors or insurers — are at the heart of a heated and ongoing debate.
Get it in writing. Pat Palmer, founder of Medical Billing Advocates of America, suggests getting confirmation documents from your doctor and your insurer before surgery. That means a prior authorization letter from your insurer and confirmation in writing from your doctor that he or she plans to perform the same procedure.
Also, Palmer says, official reports that document the details of a surgery can either help to overturn a denied claim or, if it was underpaid, increase reimbursement. Request that your surgeon’s office send the report to your insurer if there is a problem with your claim.
Know the code. The procedural codes associated with your surgery should appear on the pre-authorization letter you receive from your insurer. It’s critical that what is billed by your healthcare providers matches the procedure your insurer approved.
“You need to look through the various levels of care provided and make sure that they were aligned with prior approval,” says Nicole Evans, spokeswoman for the California Assn. of Health Plans, which represents 40 health plans insuring more than 21 million Californians.
It’s quite common that diagnosis and/or procedure codes submitted by your providers for the care you received don’t match those used to gain approval for your surgery in the first place, which will result in your claim being denied.
So your first step is to make sure a simple coding error isn’t the cause of your insurer’s refusal to pay. If it is, have your provider resubmit the claim with the correct codes.
Confirm your insurer is up to date. Coverage was denied after Altschuler’s back surgery for a number of reasons. Among them, he says, was that his surgeon used a device during surgery not approved by the FDA for that purpose.
Altschuler says he had no knowledge ahead of time about this, and he obviously would have no say in his doctor’s choice of treatment during the surgery.
“No patient is going to know the medical decision doctors make about which knife or tool is used and [patients are] at the total mercy of the provider,” Palmer says. In that case it should be the provider who is financially penalized, not the patient.
“The doctor wasn’t forthcoming about something that’s a financial burden to the patient,” Palmer says. And that case should be made to the insurance company.
But the problem can sometimes be outdated information. “Many times insurers say something isn’t FDA approved, and when investigated the insurer’s system hasn’t been updated. It may have been approved six months ago. Investigation into that can overturn the decision,” Palmer says.
You can ask for your provider’s help in gathering information or collect medical journal articles that support the treatment’s use by searching journal articles with PubMed, a service of the U.S. National Library of Medicine, at www.pubmed.gov.
Appeal to your insurer. Both state and federal law entitle you to at least two levels of appeals — an internal appeal with your insurer and a review by an independent third party.
Palmer recommends requesting a live appeal, either by conference call or in person. “When you send in [your appeal], you don’t know who is looking at it, but if you do it live it can be discussed,” she says.
Also, ask that your healthcare providers place your account on hold while you work things out. “You want to avoid having the bill sent to collections,” says Erin Moaratty, spokesperson for the Patient Advocate Foundation in Hampton, Va. “They’re usually happy to do that as long as there is something actively going on” with billing, she says.
And, of course, you have the right to retain the services of an attorney, which after eight months of fighting is the route Altschuler has gone.
“We’ve submitted countless numbers of records and opinions and MRIs,” he says of the work he and his attorney have done. “The best news out of all of this is I’m fine,” he says. “I’m even in better physical shape than before the surgery.”
Resources and links:
HMO appeals and general consumer assistance: California Department of Managed Care: (888) 466-2219 or healthhelp.ca.gov.
Insurance appeals: California Department of Insurance: (800) 927-HELP (4357) or www.insurance.ca.gov.
Employer-funded health plan appeals: U.S. Labor Department at (866) 444-3272 or www.askebsa.dol.gov.
Zamosky is the author of a new book, “Healthcare, Insurance, and You: The Savvy Consumer’s Guide.”