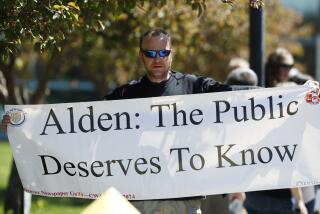
Medicare extends coverage for obesity
Medicare, the nation’s medical safety net for seniors, on Wednesday announced it would extend its coverage for obesity screening and “intensive behavioral therapy,” ensuring that roughly 30% of the 42 million people insured by the program can undertake a weight-loss program supervised by their doctor.
The decision by the federal government to cover face-to-face doctor visits as an aid to weight loss is likely to prod private insurers, many of whom have been reluctant to cover medically supervised obesity treatments, to follow suit.
Medicare‘s decision will permit beneficiaries -- typically those 65 and older -- to see a physician once a week for a month for obesity counseling, then once every other week for an additional five months if they have a BMI calculator” href=”https://www.nhlbisupport.com/bmi/” target=”_blank”>body mass index above 30 -- the standard definition of obesity. If the beneficiary loses three kilograms or more -- 6.6 pounds -- in that period, Medicare will approve an additional six monthly doctor visits for further counseling.
The federal decision “is an important step in aligning Medicare’s portfolio of preventive services with evidence and addressing risk factors for disease,” said Dr. Patrick Conway, chief medical officer of the Centers for Medicare and Medicaid Services. It comes as obesity and obesity-related diseases threaten to drive healthcare cost increases for the nation’s most costly health insurance funded by taxpayers, with current yearly expenditures of more than $325 billion.
The problem: While research finds that physician counseling can be a powerful prod to weight loss for those who need it, many physicians have been reluctant to offer it. While some of that reluctance has stemmed from an absence of insurance reimbursement for such services, many also cite patient pushback and a lack of effective tools as reasons for shrinking from the task of identifying obesity, counseling patients about its health hazards and getting them started on a weight-loss program.
With the latest decision, they are certain to see continued pushback from the nearly 13 million obese patients on Medicare’s rolls, and they remain at a loss for prescription drugs to offer. But they are likely to find some useful advice to offer as obese Medicare patients line up for treatment.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.