A detour on health reform
The healthcare reform law passed last year requires insurers to offer, at a minimum, a set of “essential” benefits to individuals and small groups, including coverage for hospitalization, outpatient care and prescription drugs. The details of what is or is not essential were left to the Department of Health and Human Services to decide.
On Friday, however, the department put out a bulletin proposing to let each state come up with its own definition. The move — which shielded the administration from a potential firestorm of criticism from patient advocates on one side and business groups on the other — was politically deft. But creating a patchwork of 50 different standards for health coverage would be bad policy. Administration officials now say the move is merely temporary, and it had better be.
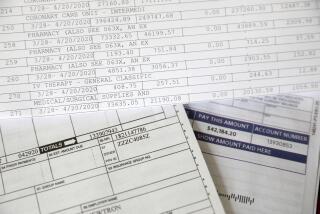
The Patient Protection and Affordable Care Act called for insurers to offer a standardized minimum benefits package to make it easier for consumers to shop for plans and to reduce the number of people with inadequate insurance policies. The latter problem contributes to the high number of Americans forced into bankruptcy by medical bills. The law lays out 10 categories of services that must be covered, but also says benefits must mirror “a typical employer plan.”
Creating such a standard is no easy task. As an Institute of Medicine panel noted, defining essential benefits the right way — considering effectiveness as well as coverage — is crucial to controlling costs. Doctors and patient advocates want to maximize coverage, while insurers and employers want to minimize it in order to limit costs. In addition, some states currently require insurers to cover more medical services than others. Coming up with one national standard would result in some states’ residents receiving (and paying for) broader coverage than they now have, with other states potentially having to mandate fewer benefits.
The administration ducked those questions. The HHS bulletin calls on states to define their own essential benefit plans, using as a benchmark one of the most popular insurance plans being offered in their state. Federal officials argue that there’s not a great deal of difference across the country among such plans, or in their cost. One problem with that argument, though, is that the law states that HHS “shall define the essential health benefits.” That’s a clear call for a national standard.
There’s also a question of fairness. Because the law requires the federal government to provide subsidies to make the basic policy affordable for the working poor, a state that defines more benefits as “essential” will draw larger federal subsidies.
The bulletin released by HHS says the agency will reevaluate its approach in 2016, although it doesn’t commit to establishing a single national standard at that point. It should. Postponing the battle over essential benefits may buy time for states to focus on other important requirements of the law, such as creating an exchange for the uninsured to shop for policies. But Congress was right to call for a national standard, and the sooner HHS can develop one, the better.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.