Once harmless, the Zika virus became lethal after a single genetic mutation took hold around 2013

When the Zika virus was first isolated from a Ugandan forest monkey in 1947 and found in mildly ill humans a few years later, it was hardly worth a mention in the annals of human disease.
What a difference a mutation can make.
In a new round of genetic sleuthing, Chinese researchers have pinpointed the single genetic change that has made the Zika virus a fearsome plague to pregnant women and their babies across the Americas, responsible for thousands of cases of microcephaly and other grievous brain abnormalities that sometimes result in death.
The Chinese researchers also came close to pinpointing the time at which the Zika virus graduated from unwelcome pest status to an international scourge. That change, they surmised, occurred around May 2013, a few months before the start of a two-year outbreak in French Polynesia and three other Pacific islands.
By March 2015, the Zika virus had arrived in Brazil and was circulating widely there. As of last week, it had caused microcephaly and other grievous brain abnormalities in at least 3,589 babies born to women infected during pregnancy, including 2,952 in Brazil.
The findings were reported Thursday in the journal Science.
As Zika hopscotched across the world, borne by soccer players and other world travelers, its genetic blueprint — RNA — underwent a number of changes. The new research underscores how that entirely normal process of genetic “drift” can, at any moment, change the trajectory of human history.
Genetic mutations picked up along its journey can disarm a virus as a threat to humans. Or, they can equip it with virulent new powers to sicken. Often, these mutations do nothing at all.
The recorded history of the Zika virus posed a mystery for modern-day public health researchers and officials.
Upon entering a human body, had the long-unheralded flavivirus always had the power to attack any developing brain tissue inside its human host and wreak a special kind of havoc? Had that destructive power simply not been picked up because previous outbreaks were too small, or included too few pregnant women?
Or had the Zika virus acquired an ominous mutation before hitting the Americas?
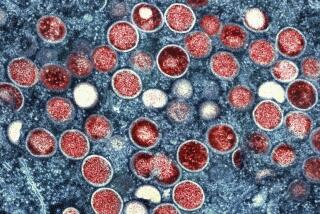
To find out, researchers from the Chinese Academy of Sciences tested a collection of Zika virus samples taken over time to see how their genetic structure had changed.
Comparing strains harvested in 2015 with one collected in Cambodia in 2010, they identified seven sites where the virus’s RNA had changed. Each change altered Zika’s surface protein by just one feature — a single amino acid.
Team members created cloned cells bearing each of those genetic alterations and used the resulting strains to infect fetal and newborn mice.
The researchers suspected they had their culprit when a cloned Zika strain bearing a mutation at position S139N of the virus’s RNA caused “strikingly” greater destruction in the brain cells of newborn mice, whose neural development mimics that of human babies during the second trimester.
Then they infected human neural progenitor cells — the forerunners of mature human brain cells — with the Zika strain bearing that single mutation. Compared to the 2010 Zika strain, the mutated version grew and multiplied more prolifically, becoming a ruthless killer of brain cells.
The researchers had found their mutation.
“The fact that this change in behavior can be almost wholly attributed to a single amino acid change in one of the virus’ surface proteins is remarkable,” said Jonathan Ball, a molecular virologist at the University of Nottingham who has probed genetic shifts in the Ebola virus.
“This data, as well as evidence from other viruses like Ebola, shows us that the smallest of genetic changes can have a major impact on virus behavior,” Ball added.
The Zika virus’s penchant for attacking developing brain tissue has come into increasing focus in recent research.
Earlier this month, a team of U.S. researchers publishing in the Journal of Experimental Medicine found that Zika may spare normal adult brain tissue, even as it seeks and destroys the primitive cells which, in a fetus, give rise to the brain’s diversity of cells.
The U.S. National Institute of Allergy and Infectious Diseases has supported much of the research that has characterized the Zika virus, though not the genetic research out this week. NIAID’s director, Dr. Anthony Fauci, called the new report a “very elegant molecular study.”
The findings from China underscore the importance of tracking not just a virus’s journey across a human landscape, but also the molecular changes it undergoes along the way, he said.
“This adds insight into our understanding of the world of viruses,” Fauci said.