Veterans protest the gutting of West L.A. PTSD therapy groups

Dov Simens said he was “playing Rambo” in a homeless camp on Wilshire Boulevard 34 years ago when he stumbled on a therapy group for combat veterans with post-traumatic stress disorder.
Through weekly sessions on the West Los Angeles veterans campus, Simens, 75, a member of the military’s secretive Phoenix interrogation and assassination program in Vietnam, was able to marry, have children and buy a house in Sherman Oaks, he said.
Buoyed by his success, he took a break. But anger and depression drove him back to the “group of my peers.”
“I have PTSD and I know that there is no cure,” Simens said. “There is no pill or opioid that will make what I did disappear.”
Now he and other veterans say the U.S. Department of Veterans Affairs has soured on long-term therapy and started dismantling the West L.A. PTSD program, which has helped thousands of former service members heal the invisible wounds of war.
Before August, about 20 groups, each with five to 30 members, had been meeting on the medical campus for a total of 40 hours a week of therapy, said Leslie Martin, the former PTSD therapy program director. The combat veterans group shut down this fall after refusing the VA’s order to move to cramped quarters with no privacy, she added.

Two other groups have stopped meeting or relocated since summer; others merged and participation is dropping, Martin said. Martin filed a whistleblower complaint over the service reductions before retiring last month. The complaint accused the VA of reassigning her to work as a clerk as retaliation for her support of veterans protesting the changes.
Citing the federal Privacy Act, VA spokeswoman Nikki T. Baker said she couldn’t address Martin’s employment.
Baker said the number of groups varies depending on demand for therapy. Seven focused on PTSD continue to meet on campus, she added.
But in a September letter protesting the shift, Rep. Ted Lieu (D-Torrance) said he understood the group therapy program was being replaced by “evidence-based” treatment — 12-week courses of specialized talk therapy that have been shown to be effective for PTSD treatment. Once open-ended, the groups would be available only for the duration of the courses, Lieu said.
“It is important that we maintain a host of treatment options for our veterans suffering from PTSD,” he said.
The secretary of Veterans Affairs, Robert Wilkie, responded that the group therapy program was being “rebranded,” not ended. But he also questioned the effectiveness of group therapy for veterans with PTSD.
“Despite the popularity and long history of support groups as routine care for veterans with PTSD and trauma exposure, there is no strong evidence that this modality is an effective treatment,” Wilkie said in a letter to Lieu.
The outcry comes at a difficult moment for the veterans agency, which is experimenting with privatizing mental healthcare while also grappling with staffing shortages and a suicide crisis — 20 former service members a day take their own lives.
Several former clinicians have complained to the VA about an exodus of as many as 50 psychologists and psychiatrists from the Greater Los Angeles VA Health Care System, which includes the Sepulveda and West L.A. campuses.
The VA says PTSD affects 8% of veterans. The agency initially relied on medication to treat the condition, but now is turning to short-term, evidence-based therapies, including cognitive processing, prolonged exposure and eye movement desensitization and reprocessing.
Cognitive processing helps veterans recast negative thoughts about their trauma. Prolonged exposure guides veterans into reliving traumatic events to diminish their fear and anguish, and eye movement desensitization and reprocessing helps veterans recall their trauma while focusing on external motion or sound.
Each therapy course generally runs for three months. Martin said VA officials made it clear they like evidence-based treatment because it’s short and saves money. VA leaders called the therapy groups “social clubs” and said veterans who need more support should take each other’s phone numbers, Martin said.
Evidence-based therapies can be tough on veterans, who may have spent years trying to forget the very memories that the sessions dredge up. In his letter, Lieu said only 50% to 60% of veterans complete evidence-based therapies.
Peter Erdos, 35, said he tried medication and evidence-based therapies with minimal success after his return from Iraq.
“Medication is something that the VA was OK with me being on for the rest of my life,” said Erdos, a member of the combat veterans group. “Coming back in my 20s and hearing that was just soul-crushing. What worked for me was camaraderie with the guys.”
Research on the effectiveness of group therapy to treat combat veterans with PTSD is inconclusive. Carl Castro, director of USC’s Center for Innovation and Research on Veterans & Military Families, said the VA should have studied the groups before squeezing them out.
“The VA has gobs of money to do research,” Castro said. “It was a unilateral decision and goes against patient-centered therapy.”
“For a lot of veterans involved in group therapy, just the fact they’re engaging in it is therapeutic for them,” said Paul Brown, adjutant of the American Legion, Department of California. “If it makes a difference in even one veteran’s life, we’re going to push to have it continued.“
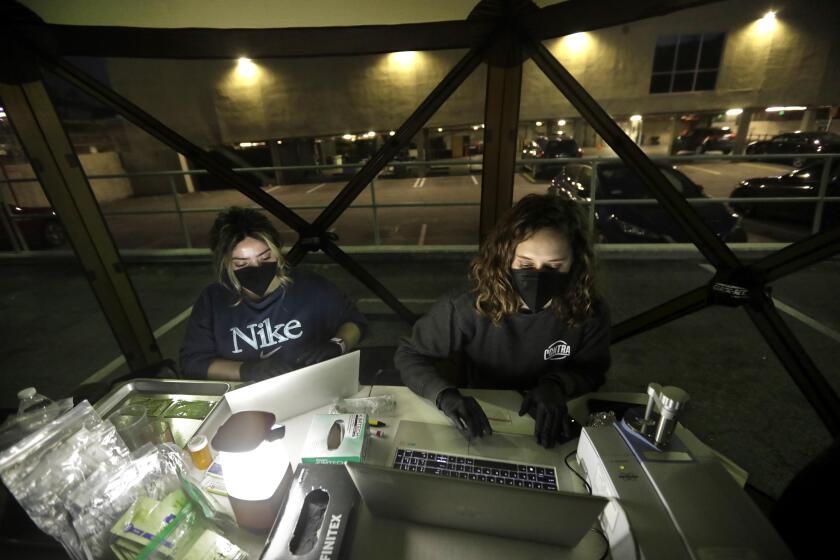
Members of the PTSD combat support group have continued meeting in a room they rent at a Westside senior center. Martin is volunteering to facilitate.
Before a gathering last month, a dozen veterans described the group as a lifeline. The men are black and white, former officers and draftees, and at least one attended West Point. Some spent years battling alcoholism or substance abuse. Some worked as lawyers, company executives or architects.
Several said they had PTSD symptoms — anger, anxiety, depression — for decades before seeking treatment.
“It only took me 47 years,” said Steven Goldstein, 71, a U.S. Army infantry veteran who served in Vietnam. “I had no joy in my life.”
Randy Kline said he was drafted out of Inglewood in 1967 “to participate in crimes against humanity“ — a moral injury that experts increasingly consider to be as damaging as a gunshot wound or other combat trauma.

Arnold Hudson said that as a black man from South Los Angeles, he saw no future as a convicted draft dodger. So he reluctantly answered the call to Vietnam, where he saw his friend “incinerated before my eyes.”
AHudson said the group gave him his life back after years of drug addiction.
“I’m 69 years old and I lost a whole lot of life,” he said. “When they announced we were disbanding I thought, why in the world is the government who vowed to take care of us cutting us off at the knees?”
The veterans said they want to return to the VA campus, where the next person home from Afghanistan or Iraq could wander in and find the support that only comes from shared experience.
“We’re a band of brothers. We have a duty to all vets,” Simens said. “We’re just asking for a 400- to 500-square-foot room, for two hours, once a week.”
Twitter: @geholland
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.