Study: More breast cancer patients should keep their healthy breasts
Too many women with breast cancer are sacrificing too many healthy breasts for too little benefit, new research suggests.
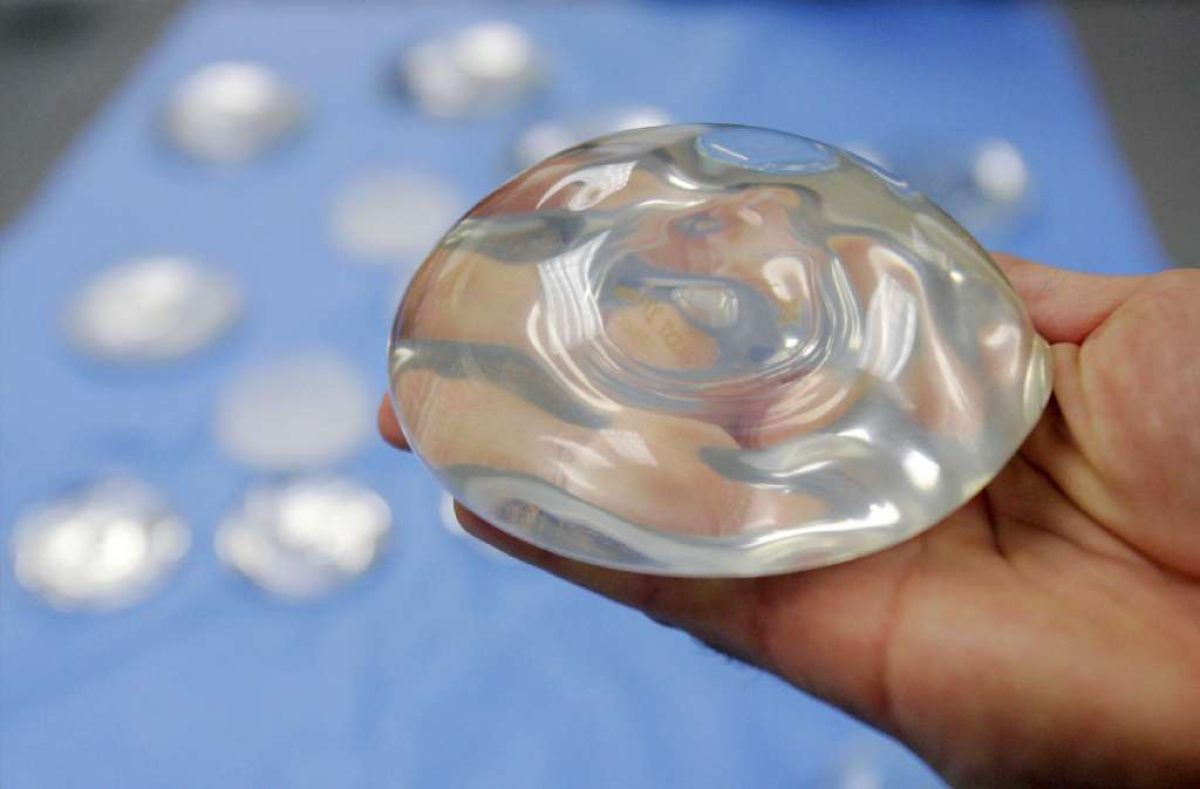
After learning that they have an early stage cancer in one breast, some women decide to remove not only the affected breast but the other one as well. Many patients believe that they can reduce their future risk of breast cancer by having the procedure, which is called a contralateral prophylactic mastectomy. (In addition, some may think they’ll get a better result with breast reconstruction surgery if they have both breasts worked on at the same time.)
In reality, women who opted for CPM did not live longer than women who decided to treat their cancers with more conservative breast-conserving surgery and radiation treatment. Data on 189,734 breast cancer patients from California show that the 10-year survival rate for women who had both breasts removed was 81.2%, according to a study in Wednesday’s edition of the Journal of the American Medical Assn. That was statistically indistinguishable from the 83.2% 10-year survival rate for women who had breast-conserving surgery and radiation. (Both groups fared better than women who opted for a single mastectomy; their 10-year survival rate 79.9%.)
And yet, the popularity of CPM is growing at a rate of 14% a year, the JAMA study found. In 1998, only 2% of women whose breast cancers were Stage 0, Stage 1, Stage 2 or Stage 3 decided to have both breasts removed. By 2011, that figure was 12.3%.
“The increase in bilateral mastectomy use despite the absence of supporting evidence has puzzled clinicians and health policymakers,” wrote the study authors, who were from the Stanford University School of Medicine and the Cancer Prevention Institute of California. “Although fear of cancer recurrence may prompt the decision for bilateral mastectomy, such fear usually exceeds the estimated risk.”
Some types of women were particularly likely to choose CPM, the study found. For breast cancer patients under age 40, use of CPM rose to 33% from 3.6% over those 13 years. Patients who were white and lived in neighborhoods with higher socioeconomic status were also more likely to have CPM instead of breast-conserving surgery with radiation. There were also some medical factors associated with a propensity to choose CPM, including having a larger tumor and evidence that cancer cells had spread to the lymph nodes.
But even when they considered these factors, the researchers still found that the more aggressive treatment option did not result in better survival. Mortality rates were “similar” for women who had CPM and those who had breast-conserving surgery with radiation, except for patients who had passed their 65th birthday – in that age group, women who had the conservative treatment fared “slightly better” than women who had CPM, the study authors reported.
“The risk-benefit ratio of bilateral mastectomy warrants careful consideration and raises the larger question of how physicians and society should respond to a patient’s preference for a morbid, costly intervention of dubious effectiveness,” the researchers concluded.
In a commentary published alongside the JAMA study, Dr. Lisa Newman said the study should empower doctors to steer their patients away from unnecessary mastectomies.
“When faced with a new breast cancer diagnosis, many patients assume that they will achieve a survival advantage by pursuing the most aggressive surgical strategy,” wrote Newman, the director of the University of Michigan’s Breast Care Center. “Patients presume that this operation represents their best chance for cure from the known cancerous breast while also eliminating a perceived inevitable threat posed by the unaffected breast.” But the findings in California “refute these assumptions,” she wrote.
For more news about the latest medical research, follow me on Twitter @LATkarenkaplan and “like” Los Angeles Times Science & Health on Facebook.