A World of Hurt : We’re feeling more pain than necessary, experts say. Laws to prevent drug abuse have doctors wary, and patients don’t know to ask about medication options. But relief may be in sight.
It is one of medicine’s great paradoxes: Pain, among the most treatable of conditions, is among the least treated. In a nation with the most sophisticated medical care in the world, many experts say they find it mind-boggling that the comfort of people in pain has been given such a low priority in medicine.
For the second time in three years, the federal Agency for Health Care Policy and Research has sharply criticized pain management practices in the United States--once again raising concerns on how pain is handled.
“I think everyone on the panel was very frustrated to know that in 1994--with this many advances that have occurred in other areas of treatment--we still have such an enormous problem with pain,” says Betty R. Ferrell, an associate research scientist at City of Hope National Medical Center in Duarte and a panel member.
Nationally, studies show that up to 50% of acute pain is under-treated. (As many as 2 million Californians needlessly suffer from acute or chronic pain.) As a result, the healing process is slowed, hospital stays are lengthened and the size of medical bills increased.
As with the panel’s 1992 report--which recommended several improvements in treating pain after surgery or trauma--no one was spared criticism in the most recent report:
* Consumers were faulted for being unaware that pain can and should be treated.
* Health professionals often receive little training in pain assessment and management.
* Laws to thwart drug abuse and drug trafficking prevent doctors from prescribing enough medication to help their patients.
But, for the first time, Ferrell says, there is progress on all three fronts.
The Law
The story goes like this: A New York state oncologist was prescribing a large supply of narcotics to a cancer patient in the course of a long, horrid illness.
But state regulators, who monitor the prescription of narcotics and other potent drugs, were suspicious of the doctor’s heavy use of the prescription pad. The authorities called the doctor to a hearing.
“The physician showed why the patient needed these amounts of drugs, and the (authorities) still reprimanded the physician,” says Ada Jacox, a pain expert at Johns Hopkins University who is familiar with the case.
This kind of case, she says, has “a chilling effect. Doctors are then conservative about prescribing enough medication.”
California is no exception to this predicament. But, recently, in a ground-breaking meeting, medical experts and state lawmakers met to try to resolve one of the thorniest issues in pain management: How to stop drug abuse and illegal trafficking but ensure that patients in pain get appropriate relief.
“Studies show doctors tend to reduce the use of more potent drugs and go to less powerful drugs” when faced with prescription monitoring, Jacox says. “And you are dealing with a situation where patients are already under-medicated.”
In California and a few other states, doctors are required to use triplicate prescription pads for narcotics; a copy is filed with the state Bureau of Narcotics Enforcement for monitoring purposes.
Studies have shown that when triplicate laws are enacted, prescriptions for narcotics drop 50%. While doctors are still free to prescribe the drugs, many are uncomfortable that the state is looking over their shoulders, Ferrell says.
“It’s a very significant problem,” she says. “This is an example of how a very compassionate physician who wants to provide pain management faces a barrier.”
In the past year, discussion has turned to whether to rescind California’s triplicate prescription law.
Milton Shoquist, a representative of the Drug Enforcement Administration in Fresno, says physicians in California are rarely called on to justify their prescriptions. Even so, the triplicate system helps to deter the misuse of drugs for illicit purposes, he says.
But a study by David Joranson of the University of Wisconsin found that “it’s not very conclusive that states with triplicates do a better job on drug diversion.”
Although “there is a great deal of hesitation” to give up triplicate prescription, an alternative that may benefit both patients and law enforcement agencies is within reach, says Bill Marcus, liaison counsel for the California Board of Pharmacy.
The alternative is a computer system connecting pharmacies to a state office where prescriptions could be monitored electronically. The system would be more convenient for doctors ordering narcotics by lessening the paperwork and might ease some of the stigma.
Health Care Providers
He never imagined it would be this bad.
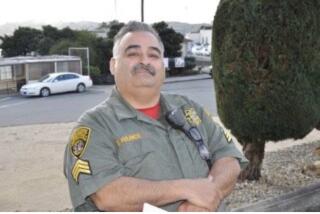
Don Russell was undergoing the first of 26 radiation treatments for throat cancer, and he was in unbearable pain.
“It felt so bad that I almost lost my mind,” recalls Russell, who was treated at the City of Hope. “The radiation melted my throat, melted the tissue together. The skin was gone from ear to ear, from my clavicle to my chin.”
When his oncologist saw how miserable Russell was, he quickly called in the hospital’s pain management team.
Having his pain brought under control was, Russell says, the most important part of his fight against throat cancer. Without the swift, effective treatment by the pain team, he could not have endured more treatments.
“Their personal attention to my problem was constant and effective,” says Russell, 62, of Visalia. “That allowed me to make a decision concerning my treatment. When you are in the degree of pain that I had, you can’t walk in and say, ‘Do that to me again.’ I received (pain medication) sufficient to allow me to make a proper decision to go ahead with the treatment.”
But the “pain team” that aided Russell is still a rarity in most hospitals. Moreover, even with electronic monitoring of prescriptions, many physicians would be reluctant to prescribe narcotics to help patients in intractable pain, experts say.
A survey of medical board members across the United States found that 25% of the doctors regarded the use of opiods as “illegal and unacceptable,” says Joranson, a survey author. Opiods, such as morphine and Demerol, are commonly needed to alleviate severe pain.
The survey shows that some doctors fear the medications even more than laws governing their use.
Because many physicians lack knowledge about pain medications, overturning the triplicate program won’t solve all cases of under-treatment of pain, warns Dr. H. Westley Clark of the Department of Veterans Affairs Medical Center in San Francisco.
“If the attitude is that the physician should not prescribe narcotics, then any prescription for narcotics is going to be unacceptable. Doctors’ attitudes and knowledge about pain must change,” he says.
“Pain has never been considered a health care problem in its own right,” says Jane Cowles, author of the new book “Pain Relief.”
“It has never been part of the standard medical school curriculum despite (doctors’) moral, ethical and legal mandate to relieve pain.”
The lack of expertise is discouraging because it is possible to treat most pain, even the most severe pain, says the City of Hope’s Ferrell.
“There is a saying that the relief of cancer pain awaits no scientific breakthrough. We have the answer, and that is one of the things that makes (the failure to treat) most frustrating,” she says.
Health professionals are still affected by many myths and biases that interfere with effective pain management, Cowles says, such as the fear of addiction--which studies show is unfounded--and the doctor’s preset notion about how much discomfort a procedure or disease should cause.
Hospitals and clinics are also being encouraged to develop specific plans for pain management and to appoint pain specialists in their facilities.
The Joint Commission on the Accreditation of Health Care Organizations, which reviews hospitals for accreditation, has also begun to look at pain. The agency is surveying hospitals on their pain-management practices and may add a pain-management requirement to the accreditation criteria.
Medical and nursing schools are also coming under pressure to augment their teachings on pain. Nursing students receive an average of 3.9 hours of time on pain management, according to a study by Ferrell. Another study found that the average medical student has one hour of study on pain.
“You can see this gap between what we are taught formerly in school and actual practice where every day you encounter patients in pain,” Ferrell says. “If we don’t start educating nursing and medical students, we can’t make effective progress.”
The Patient
Consumers also need education on pain treatments, experts say. But, unlike some health professionals, patients seem eager to embrace a more activist role, says Jacox, co-chair of the recent cancer-pain guidelines.
When the Agency for Health Care Policy and Research released its first report on pain management in 1992, it was deluged with requests from consumers for the document, Jacox says.
Ferrell, however, thinks consumers are still too timid to ask for the pain management they deserve, in part because they too have misconceptions about pain.
“The No. 1 barrier is educating patients and families so that they know to expect pain management,” she says. “People expect pain and they don’t understand that something can be done about it.”
Moreover, patients unreasonably fear drug addiction or side effects from medication. Or they resist taking medication “too early” because they think it won’t work later. And, in some cultures, not being able to withstand pain is a sign of weakness.
Opiods and other strong medications do carry the risk of side effects, such as sedation, constipation or even allergic reaction. The risk of becoming addicted, however, is extremely small--about three-hundreds of 1%, according to one oft-cited study.
What needs to happen, Ferrell says, is the kind of movement in the 1970s and ‘80s that led women to demand control over their pain-relief options during childbirth.
“I think change is coming and patients are going to start seeing written materials on what they can do,” she says. “It’s a growing movement. Obviously, we have a lot of work to do.”
Consumers need to expect adequate pain relief in the same way they expect competent overall care, Cowles says.
“People need to be reassured that 90% of all pain can be alleviated,” she says. “And if their doctor is not actively trying to do that, they are not getting the best care possible.”
Patients should be told of the many options to relieve pain, Cowles says, including exercise, support and relaxation as well as medications.
New tools have been developed to help people communicate about pain, such as numerical scales for patients to rate their pain, and diaries to keep track of the patterns of pain and what relief measures work best, Cowles says.
But, for now, patients will have to become activists.
“It’s not going to come from the top down,” Cowles warns.
“It’s going to be the consumer who learns how to ask for it. When the consumer starts asking for the care they deserve, it will start happening.”
Information on Pain Management, Federal Guidelines
* The new federal guidelines from the Agency for Health Care Policy and Research can be ordered by calling (800) 4-CANCER. The guidelines are free.
* The City of Hope National Medical Center has free handbooks: “Patient Handbook for Cancer Pain Management” (for adults) and “Your Child’s Comfort: A Team Approach to Managing Your Child’s Cancer Pain.”
Send requests to City of Hope National Medical Center, c/o Marketing/Public Affairs Department, 1500 E. Duarte Road, Duarte, Calif. 91010-3000.
More to Read
Start your day right
Sign up for Essential California for news, features and recommendations from the L.A. Times and beyond in your inbox six days a week.
You may occasionally receive promotional content from the Los Angeles Times.