A veil of secrecy shields hospitals where outbreaks occur
The cardiac surgeon had unknowingly spread a staph infection from the rash on his hand to the hearts of at least five patients by the time Los Angeles County health investigators learned of the outbreak.
The doctor had operated on more than 60 others in recent months, and county officials feared those patients could be struck with the same dangerous infection.
------------
FOR THE RECORD
Hospital outbreaks: In the April 19 Section A, an article about official secrecy surrounding infection outbreaks at medical centers recounted a 2012 incident involving a staph infection spread among heart patients at an unnamed hospital. The story said that the Los Angeles County Health Department identified the institution in an annual report only as “Hospital A” and that the name of the hospital remains secret. In fact, Cedars-Sinai Medical Center confirmed the incident months after it happened in response to questions from The Times.
------------
Investigators didn’t ultimately tie any deaths to the 2012 outbreak, but four patients needed additional surgery because of the infection.
The only public mention of the case came a year later in a little-noticed appendix to the health department’s 350-page annual report. It referred only to “Hospital A.” Even now, the name of the hospital remains secret.
L.A. County health officials investigate and confirm an infection outbreak inside one of the county’s hospitals once or twice a month. The public rarely finds out which hospital is involved, how many patients were stricken or whether any died.
The secrecy surrounding hospital outbreaks runs counter to the push toward more public disclosure in healthcare. In recent years, consumers have benefited from data comparing some health outcomes by hospital, the fees hospitals charge for various procedures and the payments doctors receive from drug and device manufacturers.
Keeping outbreaks confidential is a common practice of federal, state and local health investigators across the country. The rationale: It encourages hospitals to be open and quickly report suspected surges of infections.
“We rely on them to call us,” said Dr. Laurene Mascola, chief of the county’s acute communicable disease control program, though she acknowledges that the hospitals don’t always self-report.
In California, hospitals are required to report unusual events such as outbreaks to state health officials — but face no financial penalty if they don’t.
Proponents of more openness argue the secrecy can prevent hospitals from learning from one another’s mistakes. They say it also deprives patients of information they could use in choosing where to receive care.
More than six years ago, a lethal bacteria struck two hospitals in Florida, killing 15 patients. The case was nearly identical to the recent outbreaks at UCLA and Cedars-Sinai medical centers. In each case, a hard-to-clean medical scope transferred the same superbug from patient to patient.
Since that 2008 Florida outbreak, investigators have tied the same scopes to scores of patient infections in other states. Most of the outbreaks were not disclosed until months or years later, often only when doctors wrote about them in medical journals.
“When you keep it secret, other hospitals are uninformed,” said Lisa McGiffert, a patient safety expert at Consumers Union. “Public disclosure is absolutely essential.”
By keeping the outbreaks confidential, the county has been more successful in encouraging hospitals to report incidents quickly, Mascola said. The county staff works with hospitals to improve their practices and lower the chance of another incident.
The investigations are often scientifically complex. And at times, hospitals have disagreed with the county’s findings.
For example, three years ago the county investigated what appeared to be an outbreak of aggressive fungal infections caused by dust from hospital construction. Six children died.
In all, a dozen children in the bone marrow transplant unit tested positive for signs of the infections. The youngest was 6 months old. The children were all suffering from leukemia and other serious illnesses.
In three of the fatal cases, doctors listed the fungal infection as a cause of death.
The county’s findings were published months later at the end of the public health department’s annual report. The hospital was not identified, but The Times traced the case to Children’s Hospital of Los Angeles.
Outbreaks from construction dust have happened repeatedly inside U.S. hospitals, although the risk is little known to the public.
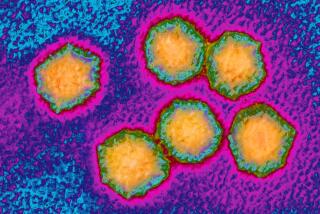
The danger comes from a common type of mold called Aspergillus. The fungus is mostly harmless to healthy people but can be lethal to those with compromised immune systems such as the children in the bone marrow transplant unit.
At the time, Children’s Hospital was building a pedestrian bridge over Sunset Boulevard. Investigators found that visitors and staff walked by the construction to get to the main entrance.
In their report, county investigators said “there were significant reasons to suggest that an outbreak occurred.”
They pointed to how doctors had listed invasive fungal infection on the death certificates of three children. Investigators also found traces of Aspergillus in 10 patient rooms.
In the end, county officials stopped short of calling the case “a true aspergillosis outbreak.” Instead they said “the most likely hypothesis” was that the patients “were exposed to a source in the environment” and “the probable source” was Aspergillus.
Children’s Hospital says that construction played no role in the deaths of the children, who were seriously ill when admitted. During the county’s investigation, the hospital’s doctors called it “a pseudo outbreak,” according to the county’s report, arguing the tests pointing to fungal infections in the children were wrong.
Doctors pointed to environmental testing by companies hired by the hospital that had found no sign of fungus in the transplant unit.
“We do not dispute the county’s report,” said Lorenzo Benet, a spokesman for Children’s Hospital, “but we want to be clear that no conclusive evidence of an outbreak was found and at no time was our institution deemed unsafe for the provision of patient care.”
Mascola, the county’s disease control chief, said officials would disclose an outbreak if they believed it would be in the public’s interest. County officials said they couldn’t immediately point to a case in which that happened.
In the recent superbug outbreak at UCLA, the university confirmed the outbreak after questions from The Times.
The same medical device — a duodenoscope — was found to be the cause of the outbreak in the Florida hospitals that began in late 2008. In both cases, the reusable scope transferred a superbug known as CRE, or carbapenem-resistant Enterobacteriaceae, among patients. The germ kills as many as 50% of its victims.
Florida officials said they discussed the outbreak with federal officials from the Centers for Disease Control and Prevention and the Food and Drug Administration in June 2009.
But there was no public disclosure of the case until Florida doctors wrote about it four years later in a medical journal. The hospitals have not been named.
Melissa Brower, a CDC spokeswoman, said it is up to state and local health officials to decide whether to tell the public about outbreaks.
Both the CDC and the FDA say they did not warn the public about the deadly Florida case because investigators found that hospital staff had failed to properly clean the scope — a long-standing and repeated problem that the agencies had already warned hospitals about. The agencies sent an additional general warning about sloppily cleaned scopes in late 2009.
UCLA and Cedars-Sinai said they had followed the manufacturers’ instructions for cleaning the scope — pointing to a problem with the device’s design that made it almost impossible to disinfect.
Peter Mendel, who studies hospital-acquired infections for the Rand Corp. in Santa Monica, said that public disclosure of the 2008 outbreak could have helped regulators conclude more quickly that the scope design was flawed. “People would realize there was accountability,” he said.
A handful of bills have been proposed over the years to require more public reporting of dangerous infections.
In 2004, the Legislature passed a bill requiring facilities to tell the public how many patients get dangerous infections in their care. The California Hospital Assn. lobbied against it, arguing that it would take resources away from nursing care, according to a legislative analyst’s report. The bill was ultimately vetoed by then-Gov. Arnold Schwarzenegger.
The group objected to a similar bill in 2005 because of the cost of compliance. That bill was approved, but without the reporting requirements.
In 2008, the state Legislature passed a law pushed by patient advocates. The bill was named for Nile Moss, a 15-year-old who got an infection in 2006 after going to Children’s Hospital of Orange County for an MRI and other tests. Nile died two days later from a superbug known as MRSA, or Methicillin-resistant Staphylococcus aureus.
Nile’s Law gave the public access to limited data on the number of patients infected during specific surgeries or other procedures at each hospital. It required hospitals to report to the state bloodstream infections caused by MRSA, three other bacterial infections, as well as a variety of surgery-site infections.
In 2011, the hospital association sued, arguing that the state was asking for more infection statistics than was mandated by the legislation. That effort was unsuccessful.
Debby Rogers, an association vice president, said the hospitals believed the state had overreached by not obtaining their comments before requiring the reporting of more infections.
“Do not make the conclusion that CHA has opposed public reporting,” said Jan Emerson-Shea, the group’s spokeswoman. If the association opposed a bill in the past, she said, “it was usually particular wording.”
Carole Moss, Nile’s mother, now sits on a state committee that advises officials on how to report and prevent hospital-acquired infections. She said she is frustrated by the hospitals’ control of the committee. The panel, appointed by the state director of public health, currently has 17 members, including 12 who work for hospitals. Only Moss and two other members represent the public.
“It’s completely out of balance,” she said. “They vote on behalf of their employers.”
In 2013, Moss proposed adding the superbug CRE to the list of hospital infections that must be reported. Only the two public members present supported it.
“All of us want to know what hospital is safe,” Moss said. “These are preventable deaths. Every day goes by, and more people die.”
Twitter: @melodypetersen
Times staff writer Chad Terhune contributed to this report.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.