Column: CVS and Aetna say their huge merger will be great for consumers. Here’s why you should be skeptical

The CEOs of drug retailer CVS and health insurer Aetna were marvelously in sync Sunday when they jointly announced their companies’ $69-billion merger deal.
The deal will “dramatically further empower consumers,” Aetna’s Mark Bertolini said. It will “create a platform that is easier to use and less expensive for consumers,” according to Larry J. Merlo, president and CEO of CVS Health. They repeated these mantras to the press in a series of joint interviews.
All that was missing was a clue to how, exactly, this nirvana of better, cheaper healthcare was to be reached. Clues to how little attention the companies have paid to that detail could be found throughout their joint announcement. “With the analytics of Aetna and CVS Health’s human touch, we will create a healthcare platform built around individuals,” Merlo said, in a masterpiece of vacuous corp-speak.
After all, Aetna doesn’t need to merge with CVS to exploit its “analytics”; ostensibly, it already has data in hand to help its customers manage their health needs, and if it needs a firm like CVS to help out, the companies could sign a contract. The announcement claims the merger will end up “helping patients avoid unnecessary hospital readmissions.” But the merged company won’t own any hospitals and isn’t planning, at least at first, to place more physicians on its payroll.
With the analytics of Aetna and CVS Health’s human touch, we will create a healthcare platform built around individuals.
— CVS and Aetna promise a consumer nirvana from their merger
The companies say that “rather than feeling lost and confused, selected high risk patients discharged from the hospital… will be able to stop at a health hub location to access services such as medication evaluations, home monitoring and use of durable medical equipment, as needed.” This would be a good thing; what isn’t clear is why CVS and Aetna have to complete a $69-billion merger to make it happen. What’s preventing CVS from turning its drugstores into “health hubs” on its own, today?
As for the “human touch” of CVS, kudos to the PR aide who came up with that phrase. Do you feel “touched” by humans when you’re in your neighborhood CVS? Me neither.
The wonders of better data and better analysis have been cited to justify previous mega-mergers, especially those between insurance companies. Way back in 2004, the merger of Woodland Hills-based WellPoint into Indianapolis-based Anthem was to produce immense savings from combining their computer systems and allowing customers’ medical data to be exploited for their benefit across the new company’s vast reach.
Never mind that WellPoint Chairman and Chief Executive Leonard Schaeffer was in line to pocket $37 million out of the deal plus a lump-sum payout ot $45 million in accrued pension rights. We’re still waiting for the technological benefits of the WellPoint/Anthem deal to appear after 13 years, and the betting here is that we’ll still be waiting for the virtues of merging Aetna’s analytics with CVS’ human touch to appear 13 years from now.
That’s not to say that data analysis won’t be beneficial for Aetna and CVS. David Anderson of Duke University, a former data manager for the University of Pittsburgh Medical Center Health Plan, outlines some of these benefits: Aetna, he observes, has served the Medicare, Medicaid, and private insurance markets, which enables it to track members’ healthcare histories as they shuttle in and out of each market.
But “there are always serious holes in the Aetna list,” he writes. “Either someone has never been on Aetna before or there was a major change in health status when that person was covered by someone else. This is where CVS comes in. There is a good chance that CVS has filled some prescriptions for people who do not show up in Aetna’s data banks.” Now they will, allowing Aetna to better set prices for its products.
“The biggest data bonanza,” he adds, “is the CVS non-prescription data tied to the loyalty card that almost everyone carries on their keychain.” That gives the merged company a window into everything from when a couple is planning to have a baby to who’s suffering a flareup of arthritis. In the right hands, CVS/Aetna might ply those people with advice on prenatal care or pain management; in the wrong hands, it could prompt CVS/Aetna to find ways to push those potentially costly patients over to competing insurers. Obviously, there’s no guarantee that the company will use its deeper insights into customers’ private lives exclusively for good.
Other positive aspects of the merger cited by Merlo and Bertolini are equally nebulous. “An entirely new health services offering available in many locations will function as a community-based health hub dedicated to connecting the pathways needed to improve health and answering patients’ questions about their health conditions, as well as prescription drugs and health coverage,” the announcement says.
What does that mean, precisely? Apparently it means the existing 10,000 CVS drugstores will “include space for wellness, clinical and pharmacy services, vision, hearing, nutrition, beauty, and medical equipment.” Some already meet this exacting standard. You can buy makeup at your neighborhood CVS. Contact lenses (vision) and wheelchairs (devices) can be purchased online. You can get a flu shot at your neighborhood CVS, and if you have the proper insurance, CVS will vaccinate you for free and bill your insurer. Obviously, the standard CVS already offers pharmacy services. If CVS is going to bring some of these online purchasing options to the retail floor, that’s progress of a sort, but it mostly means that the CVS retail location will look more like the nearest Costco.
It’s proper to note that Aetna hasn’t been a paragon of customer service in the recent past. Last year, the company announced it was pulling out of all but four of the 15 states where it was providing Obamacare individual insurance because of a business decision — it was simply losing too much money on the Obamacare exchanges. This was a surprise, given that only a few months earlier, Bertolini had committed the company to long-term participation in the exchanges, calling it “a good investment.” A federal judge ruled in January that Aetna’s rationale for withdrawing was a lie — the decision wasn’t based on profit and loss, but was designed as retaliation for a federal antitrust lawsuit blocking Aetna’s proposed $34-billion merger with Humana, another health insurer. (The judge blocked the merger.)
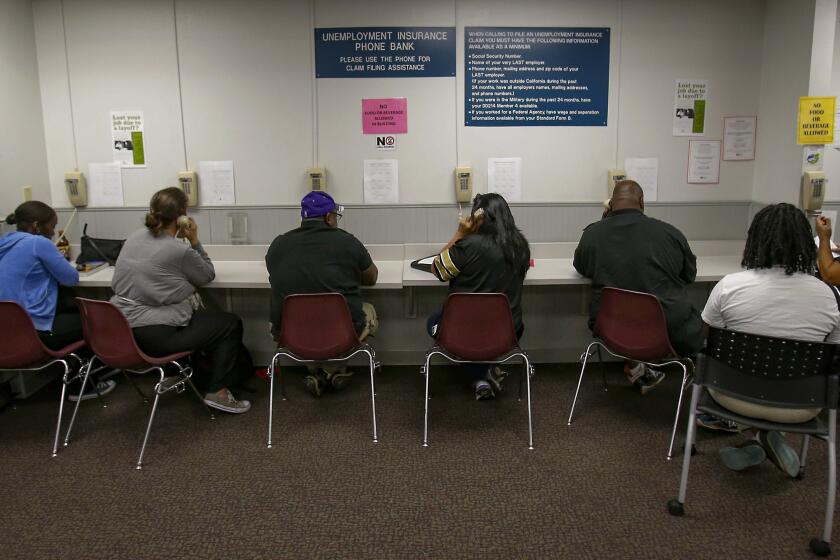
The truth is that the CVS/Anthem merger isn’t being driven by a desire to help ordinary Americans manage their healthcare costs better. It’s driven by the desire to fend off scary new competitors in the healthcare industry, such as Amazon and Wal-Mart. Will it save money? Hardly: About $8.5 billion will be transferred to Aetna shareholders from CVS (based on the $26 premium to be paid for their shares in cash and CVS stock over Aetna’s price Friday). The companies say they’ll earn some of this back by streamlining operations, which typically means cutting staff. If it’s truly redundant personnel who will be let go, the average consumer might not notice the difference; if it’s a wholesale hatcheting, that will mean less efficient services for more customers.
The evidence that the merger will lead to a “remaking” or “reshaping” of the U.S. healthcare market is scanty, not to say nonexistent. That’s because what may be the most important business affected by the CVS/Aetna deal isn’t pharmacy services or health insurance; it’s the pharmacy benefit management business.
PBMs, as we’ve reported before, emerged in the 1980s as intermediaries helping health insurers combine their customer bases for greater leverage in negotiations with drug manufacturers and to steer doctors and hospitals to cheaper drug alternatives.
Over time, however, they became just another special interest jockeying for a piece of the healthcare spending pie. The discounts they extracted from drug makers seldom, if ever, trickled down to consumers. The money went to insurers or remained with the PBM firms. Last year the big insurer Anthem complained in a lawsuit that Express Scripts, the biggest PBM, was keeping too much of the profits it squeezed from drug makers, instead of passing on a fair share to Anthem. This resembled two hyenas snapping at each other over wildebeest scraps; not much is ever left for any other species after these skirmishes.
The amount at issue was estimated as large as $15 billion, a sum any insurer would have reason to try to keep in-house. Anthem has made clear that it intends to operate its own in-house PBM in the future, instead of outsourcing the service to Express Scripts. That’s the trend that has produced the CVS/Aetna merger.
Nor would the deal be the first to bring together a PBM and a health insurer: In 2007, UnitedHealth merged CatamaranRx, then the fourth-largest pharmacy benefit manager, into its OptumRx PBM. (That same year, CVS entered the pharmacy benefit management industry by acquiring Caremark.) Are there any signs that those deals “reshaped” the healthcare market or produced savings for consumers? The short answer is no. The long answer also is no. Evidence of the profits to be reaped in the pharmacy business did attract the attention of Amazon, which is interested in moving into the market; Wal-Mart already sells drugs, often at a sharp discount from what drug chains charge.
Healthcare experts are crossing their fingers in the hope that the CVS/Aetna merger is large enough to bring rational coordination to our fragmented healthcare system. In a commentary Sunday, Austin Frakt of Boston University and the Incidental Economist healthcare blog cited research findings that coordinating pharmacy and health benefits could lead to lower costs, because a PBM that’s also “on the hook for the cost of other care”—such as through ownership of a health insurer — may be inclined to increase, rather than restrict, access to drugs that reduce overall healthcare costs.
But if the merger sets off a round of further consolidation in the PBM market, that would give the surviving companies less incentive to undercut each other by demanding greater discounts from drug companies. The result: higher prices. Despite the flowery claims offered by Messrs. Merlo and Bertolini, that’s the way to bet.
Keep up to date with Michael Hiltzik. Follow @hiltzikm on Twitter, see his Facebook page, or email michael.hiltzik@latimes.com.
Return to Michael Hiltzik’s blog.
UPDATES:
11:04 a.m.: This post has been updated with comments by David Anderson.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.