Coronavirus Today: The first shots are taken
Good evening. I’m Amina Khan, and it’s Monday, Dec. 14. Here’s what’s happening with the coronavirus in California and beyond.
It’s finally happening. The biggest vaccination campaign in American history is officially taking place now that health workers in hospitals around the country have begun baring their arms for the first round of shots designed to protect them from COVID-19. It’s the first major U.S. assault on the coronavirus, which has infected more than 16.4 million people nationally and left more than 300,000 dead.
There’s a near-palpable sense of optimism coming from doctors, nurses and other health workers who, along with nursing home residents, are first in line for inoculation. Many are weary from witnessing the devastation of COVID-19 up close, so they know just how momentous these first doses are.
The Pfizer-BioNTech vaccine was packed in dry ice as it was shipped by truck and plane from Pfizer’s factory in Kalamazoo, Mich. A buoyant Gov. Gavin Newsom tweeted, “Hope has arrived,” with a photo of himself standing in front of a freezer stocked with the precious doses.
California’s initial share of about 327,000 doses will go mostly to healthcare workers in acute-care hospitals, though some counties say they will also provide some vaccines to skilled nursing facilities.
Helen Cordova, an intensive care unit nurse at the Kaiser Permanente Los Angeles Medical Center on Sunset Boulevard, became the first Californian to get the vaccine. The needle went into her arm around 12:15 p.m. Monday, as Newsom, L.A. Mayor Eric Garcetti and other officials looked on. After each shot was administered, cheers broke out from the room of masked observers.
“I’m very excited that we have the vaccine, because it provides hope for the future,” Cordova said after getting her shot.

Pfizer received emergency use authorization from the U.S. Food and Drug Administration late Friday; authorization for a similar vaccine developed by Moderna and the National Institutes of Health is expected to follow, possibly by the end of this week. Both vaccines require two shots, given a few weeks apart. Together, the two companies will be able to deliver more than 2 million doses to California by the end of the year, and millions more in 2021.
Keep in mind that the total amount of vaccine expected to come to California by the end of the year — about 2.16 million doses — won’t be enough to cover all of the state’s 2.4 million health workers.
There are plenty of logistical hurdles to come, including delivering a second dose to everyone in the first priority group (those come three weeks later for the Pfizer vaccine and four weeks later for Moderna’s) as well as expanding the vaccination campaign to essential workers such as janitors and food handlers. Vaccines probably won’t be available to everyone who wants them until at least the spring.
In the meantime, it’s essential that we not let our guard down too soon, authorities said. Lives are still on the line as health workers continue to battle an unprecedented surge in cases. And officials say Americans won’t be able to breathe easy until we reach herd immunity, which experts say will be achieved when approximately 70% of the population is vaccinated.
“We are calling on all Californians to continue doing their part by following local and state guidance, wearing a mask and staying home,” Newsom said. “Together, we will get through this and move forward to a healthy, safer, resilient California for all.”
By the numbers
California cases and deaths as of 6:28 p.m. PST Monday:
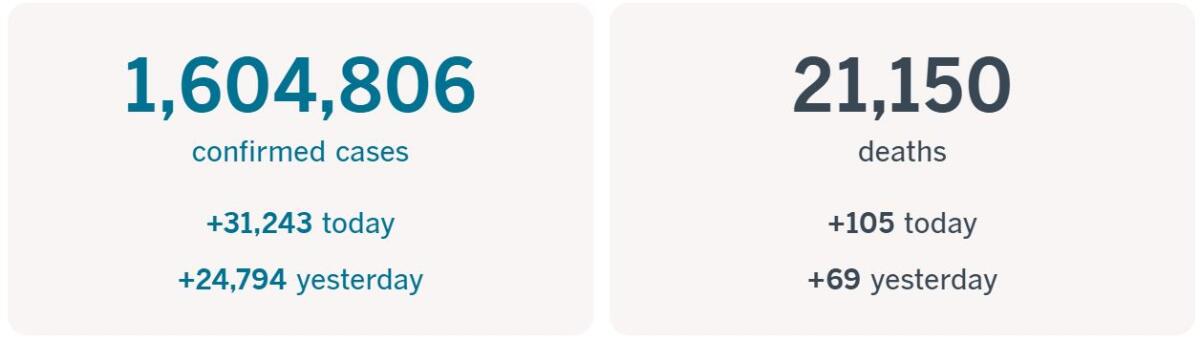
Track the latest numbers and how they break down in California with our graphics.
Across California
An estimated 4 million people have signed up for CA Notify, California’s smartphone-based COVID-19 exposure alert system, according to the state Department of Public Health. While that sounds like a big number, even more residents need to opt in for the system to be effective, officials say.
The system, officially launched Thursday, takes its cues from traditional contact tracing, in which health workers call people who’ve recently had close contact with an infected person and advise them to self-quarantine and get tested. The smartphone system sends alerts to people who were in close contact with someone who later tested positive. The hope is that if used in conjunction with traditional contact-tracing methods, the tool will help slow the virus’ spread.
Meanwhile, California is taking Amazon to court to try to force the online retail giant to cooperate with an investigation into whether the company is doing enough to protect its workers from the virus, Atty. Gen. Xavier Becerra said Monday.
“Amazon has made billions during this pandemic relying on the labor of essential workers. Their workers get the job done while putting themselves at risk,” Becerra said. “It’s critical to know if these workers are receiving the protections on the job that they are entitled to under the law.”
In a statement, Amazon challenged the legal action and said Becerra’s claims of noncompliance “don’t line up with the facts.”
Amazon said in October that nearly 20,000 of its frontline workers had tested positive or were presumed positive for coronavirus infections, but also said that the infection rate among its workforce was well below that in the general population.
In the Bay Area, Santa Clara County has begun door-to-door coronavirus testing in a majority-Latino community in San Jose that’s a hot spot for the virus. Volunteers with the pilot program started handing out self-testing kits in the East San Jose neighborhood last week, where many residents can’t easily access testing sites. Latino and Black communities nationwide have been disproportionally affected by the pandemic.
In San Diego, a surge in coronavirus cases is putting pressure on the area’s two major military hospitals. The 16 intensive care unit beds at Naval Medical Center San Diego are at 70% capacity, and three of the four ICU beds at Naval Hospital Camp Pendleton are filled.
Frontline military healthcare providers at both hospitals say that cases in the communities they serve have surged in recent weeks, just as they have in the Greater San Diego area.
“The majority of people say they believe they got it from someone close to them, like their significant other,” said Ensign Samantha Salus, a nurse in the COVID-19 ward at Naval Medical Center San Diego. “Just like our civilian counterparts, we’re seeing an influx of patients.”
Regena Kowitz, a spokeswoman for Navy Medical Forces Pacific, declined to comment on the total number of cases at the bases. “While our team is busy, the ICUs are not full,” she said, adding that both sites plan to increase patient capacity if needed.
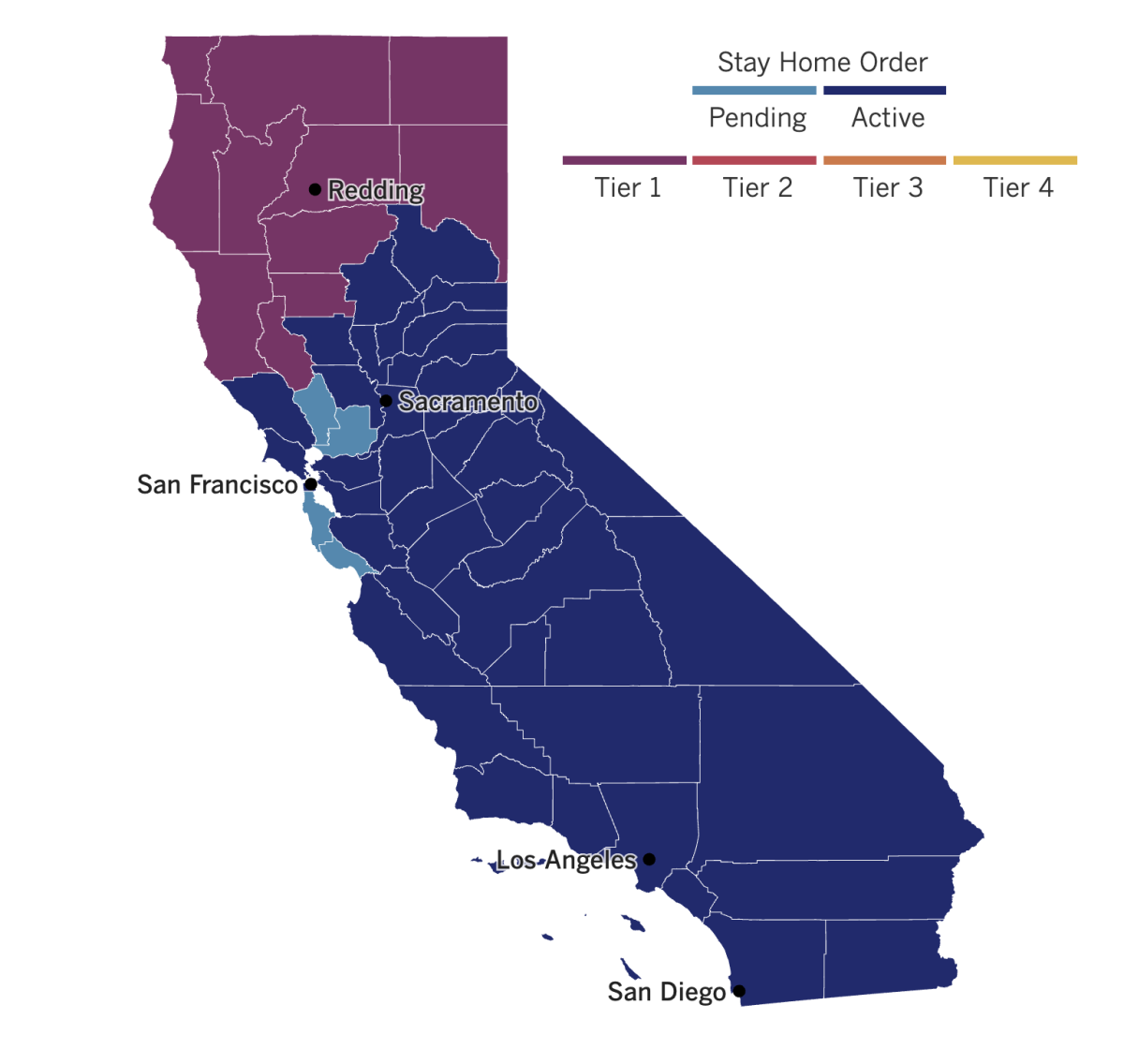
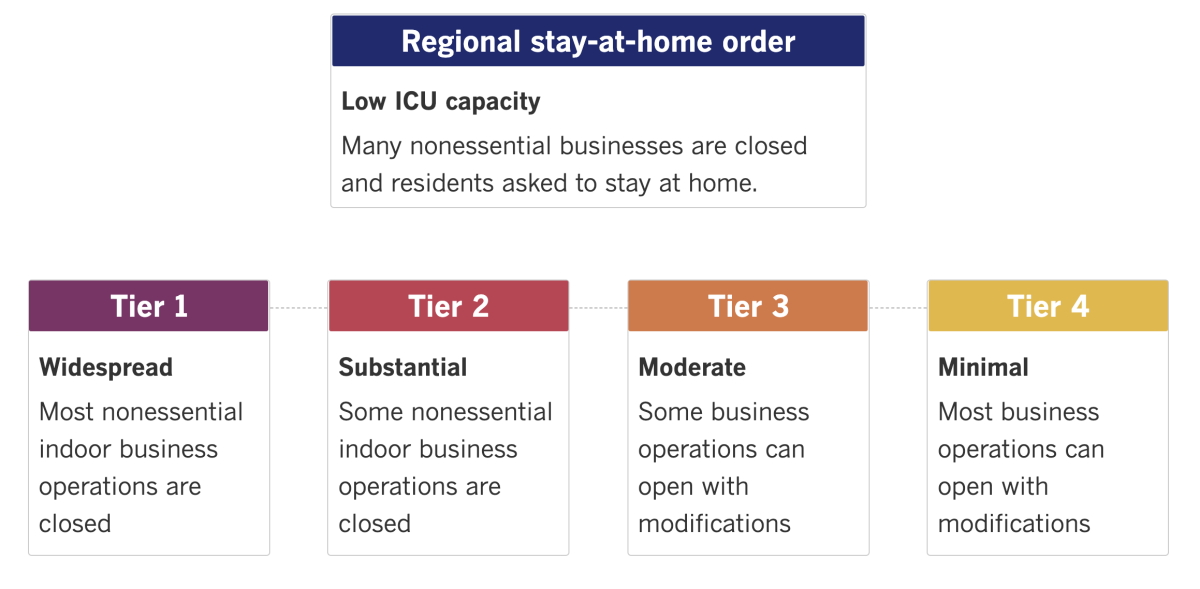
See the latest on California’s coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
March Madness, meet the pandemic. The NCAA plans to stage the full women’s basketball tournament in one geographic area, with San Antonio shaping up to be the likely host site. Officials hope the move will mitigate the risks posed by COVID-19, and it parallels the setup of the men’s tournament, which the NCAA said last month will be played in just one area, probably Indianapolis.
The women’s 2021 Final Four was already set for San Antonio. The NCAA has started preliminary talks with the city to be the home base for the entire tournament, which involves 64 teams. Nina King, the NCAA women’s basketball committee chair and senior athletic director at Duke, said the decision allows for more time to plan and put safeguards in place to protect the players.
Italy has passed Britain for another unwanted title, becoming once again the nation with Europe’s highest official COVID-19 death toll. The country was the first to be hit hard by the virus early this year, and on Sunday it logged 484 new COVID-19 deaths. While that was one of its lowest single-day counts in a month, it was still enough to push the nation’s overall death toll up to 64,520, passing Britain’s count of 64,267, according to Johns Hopkins University. (Both countries’ figures probably underestimate the true loss of life, in part because many coronavirus-related deaths were probably missed early in the crisis.)
Italian Prime Minister Giuseppe Conte has responded to the rising tally of cases and deaths by tightening travel restrictions for the period spanning the Christmas, New Year’s and Epiphany holidays. Italians will not be allowed to travel between regions except for work or urgent reasons such as health problems. On the holidays themselves, they won’t be allowed to leave their towns.
Germany, meanwhile, has ramped up its pandemic restrictions in a bid to mitigate its high infection rate. The new measures starting Wednesday will result in the shuttering of most stores, tight limits on social contacts, no singing in church and a ban on the sale of fireworks. Schools will have to close or switch to home schooling, and restaurants can offer takeout but no dine-in options. The restrictions will remain in place until Jan. 10.
The limitations come as the seven-day rolling average of new daily cases has climbed over the last two weeks from 21 new cases per 100,000 people on Nov. 28 up to 26 per 100,000 on Dec. 12.
“We are forced to act and we’re acting,” Chancellor Angela Merkel told reporters in Berlin, noting that existing restrictions imposed in November had failed to significantly reduce the number of new infections.
The United States still leads the world in COVID-19 deaths and passed the 300,000 mark on Monday, according to data compiled by Johns Hopkins University. The loss of life is more than five times the number of Americans killed in the Vietnam War, and equivalent to the population of St. Louis or Pittsburgh.
“The numbers are staggering — the most impactful respiratory pandemic that we have experienced in over 102 years, since the iconic 1918 Spanish flu,” said Dr. Anthony Fauci, the government’s top infectious disease expert.
Your questions answered
Today’s question comes from a reader who wants to know: How did the first COVID-19 vaccine get approved so fast?
The short answer is that technically, it didn’t get formally approved by the Food and Drug Administration. It was granted an emergency use authorization, or EUA, instead, as my colleague Karen Kaplan explains.
The evaluation process for an EUA is designed to be speedier than the usual FDA approval regimen so that new vaccines and medicines can get to those who need them as quickly as possible during a public health emergency. But even so, there’s a high bar for meeting those criteria.
Among other things, there have to be “no adequate, approved and available alternatives” to the product seeking authorization. And the experimental drug or vaccine must still be tested in multiple rounds of clinical trials involving thousands of participants. It has to be safe, and it has to perform better than a placebo.
Once enough data are in hand, FDA staff doctors and scientists conduct a thorough review of the study results. So does an advisory group of independent scientists and health experts. Then the agency can make a decision.
In the case of a vaccine, emergency use authorization can be granted if “the known and potential benefits outweigh the known and potential risks,” the FDA says.
In all likelihood, the coronavirus will still be circulating in the population once the pandemic ends. That means the vaccine makers will have to go through the standard approval process in order to continue distributing it.
If you want to know even more details about the process and the hurdles companies have to clear, check out the full explanation here.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them.
Resources
Practice social distancing using these tips, and wear a mask. Here’s how to do it right.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




