Experimental drug shows promise against Ebola’s cousin, Marburg virus
An experimental drug designed to halt replication of the deadly Marburg virus -- a relative of Ebola -- has proved effective in monkeys, even after they had been infected for three days, research shows.
In a paper published Wednesday in the journal Science Translational Medicine, scientists said the intravenous drug saved the lives of 16 rhesus macaques who were injected with the virus, whereas five other monkeys who did not receive the drug died within nine days.
The experiment marks the first time a drug has been shown to protect animals following infection with the Angola strain of the Marburg virus, according to the study authors, and suggests that a similar approach may be successful in treating humans infected with Ebola.
Such an Ebola treatment, according to senior study author Thomas Geisbert, a professor of microbiology and immunology at the University of Texas Medical Branch at Galveston, could be combined with another experimental drug like ZMapp to fight the virus at different stages in its life cycle.
ZMapp, which is produced by Mapp Biopharmaceutical Inc., of San Diego, is the experimental drug given to U.S. missionaries who were infected with Ebola in Liberia. Company officials say supply of the drug has been exhausted.
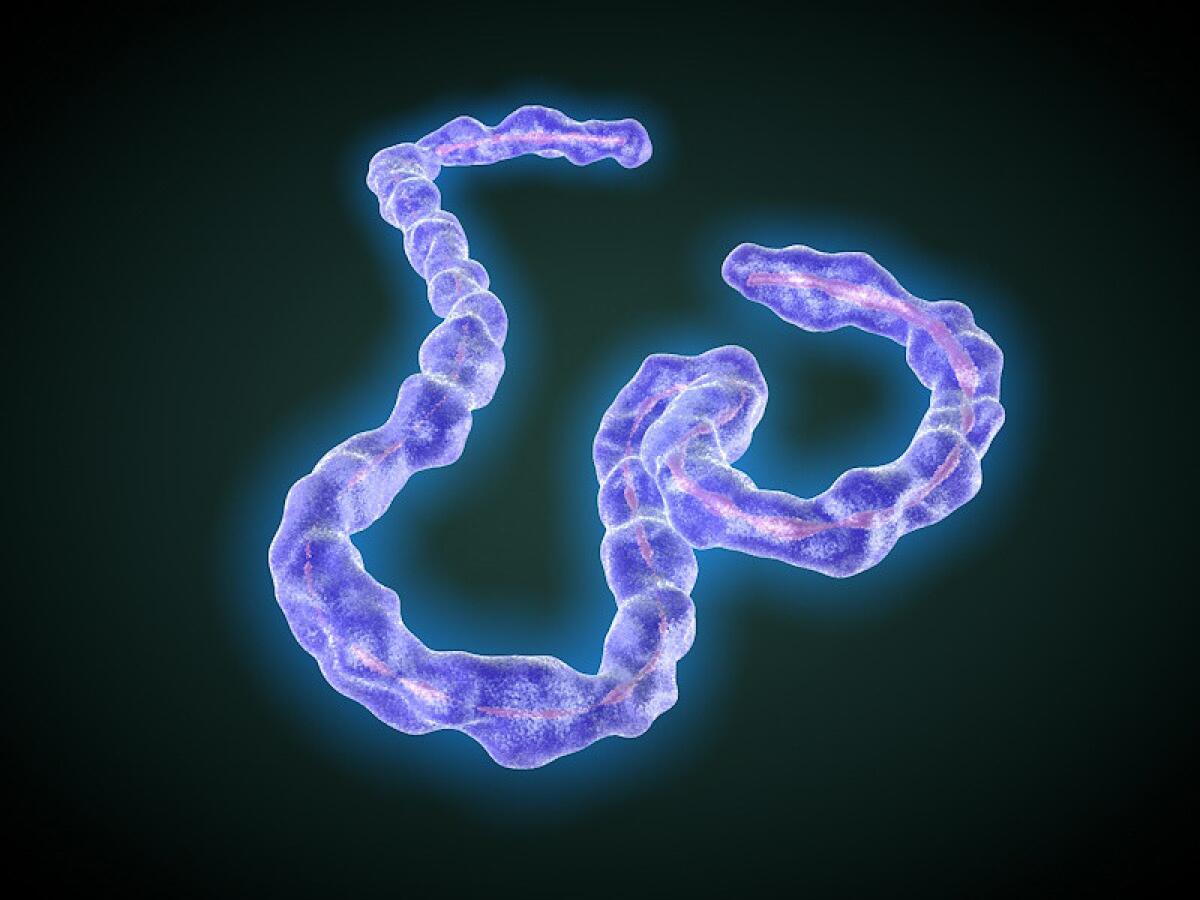
Ebola and Marburg belong to the same filovirus family and cause severe and often fatal hemorrhagic fever in humans and monkeys, as well as other animals.
Thread-like filoviruses are spread through direct contact with bodily fluids, and once they enter an organism, they attach themselves to the surface of host cells and insert their RNA into the cell. The host cell then begins making copies of the virus, which bud from the host cell and go on to invade other cells.
Within two to 21 days of infection, the virus brings on a sudden fever, severe headaches and muscle pains, which are soon followed by diarrhea, cramps and vomiting, according to the World Health Organization. After five to seven days, bleeding from the nose and gums can occur and the patient can go into shock.
Because the Marburg virus is so deadly -- it can cause death in up to 88% of cases -- it has been considered a potential biological weapon.
Though there is still no approved vaccine or treatment for filovirus infections, a number of drugs under study attempt to prevent viral invaders from attaching to cells and entering them.
However, the drug that Geisbert, his colleagues and Canada’s Tekmira Pharmaceuticals Corp. discussed in Wednesday’s paper seeks to attack the virus after it has entered the cell.
The Marburg drug consists of sections of “small interfering RNA” (siRNA), or silencing RNA, which are created in the lab and packaged in microscopic envelopes called lipid nanoparticles that can be absorbed by cells.
Once inside the cell, the siRNA hampers viral reproduction by degrading messenger RNA and shutting down the production of viral proteins.
“Maybe the best analogy I can give is the messenger RNA is a blueprint for how the virus makes more of itself, and the siRNA kind of interferes or blocks that ability for it to kind of follow its recipe to make proteins,” Geisbert told reporters during a telephone news conference recently.
In contrast, vaccines or anti-serums like ZMapp attempt to foil the virus through the use of antibodies -- Y-shaped proteins that bind to the virus and either mark it for destruction by immune cells or hamper the ability of the virus to latch onto and enter host cells.
These antibodies are much less effective once the virus has already entered the cell, however.
Study authors said it was significant that the medication worked on monkeys who had been infected for three days, because that was also the point at which they began to show symptoms.
Although the use of siRNAs appears promising in the fight against filoviruses, Geisbert said, no single drug is effective against both Ebola and Marburg.
A different siRNA that Geisbert and colleagues tested on Ebola in 2010 proved effective in treating monkeys shortly after infection, but it was not tested to see if it worked after three says of infection.
Geisbert said Tekmira had already begun Phase 1 trials on that Ebola drug to see if it can safely be used on humans.
Follow @montemorin for science news







