Thousands of L.A. healthcare workers sickened by coronavirus, worsening crisis in hospitals

The astronomical coronavirus surge in Los Angeles has infected thousands of healthcare workers in recent weeks and exacerbated the strain on hospitals struggling to care for critically ill patients.
More than 2,200 people who work at hospitals in L.A. County tested positive for the virus in December alone, constituting roughly a third of all hospital infections reported during the pandemic. Whereas in previous months nursing homes and outpatient clinics suffered the most illnesses, besieged hospitals and their beleaguered workers have been hit hardest by the winter surge.
Dr. Anish Mahajan, chief medical officer of Harbor-UCLA Medical Center in Torrance, said that adequately staffing his hospital — where the ICU is stretched to 150% of its normal capacity — is a constant challenge, with staffers out because they are ill with COVID-19 or quarantining due to exposure. Hospitals across California have reported similar trends.
“Somebody who wears their PPE perfectly and deals with high-risk patients doesn’t get sick at work. ... When they get home, their teenager might give them COVID. We see that a lot,” Mahajan said. “We end up short-staffed in everything, from nurses to doctors to even the custodial staff that helps us turn over the rooms. And all of that makes it even more difficult to take an onslaught of more and more patients.”
The recent explosion of the coronavirus has trapped L.A.’s hospitals in a vicious cycle. The more people who are ill, the more likely others will become infected, both at and away from work. That, in turn, intensifies staffing shortages at hospitals — at the very moment the public needs medical care the most.
Outbreaks have also jumped dramatically in recent months among grocery store workers and retail employees and at other workplaces. But the rise in infections comes at a crucial time for L.A.’s hospitals as they buckle under a deluge of patients and turn away ambulances, line hallways with gurneys and cram bodies into overflowing morgues.
An informal survey of LAPD employees found significant skepticism about COVID-19 vaccines, with 20% saying they’d opt out.
Officials reported Tuesday that a record 7,898 people with COVID-19 were currently admitted to hospitals in L.A. County, a record-breaking total that is expected to grow in the coming weeks.
“We’re going to continue to work with organizations across the county to ensure that healthcare workers at every location are protected,” L.A. County Department of Public Health Director Barbara Ferrer said this week.
Since the pandemic began, 28,448 healthcare workers and first responders have tested positive for the coronavirus in L.A. County, and 132 have died from the virus, Ferrer said. Hospitals, nursing homes and outpatient clinics account for the majority of cases.
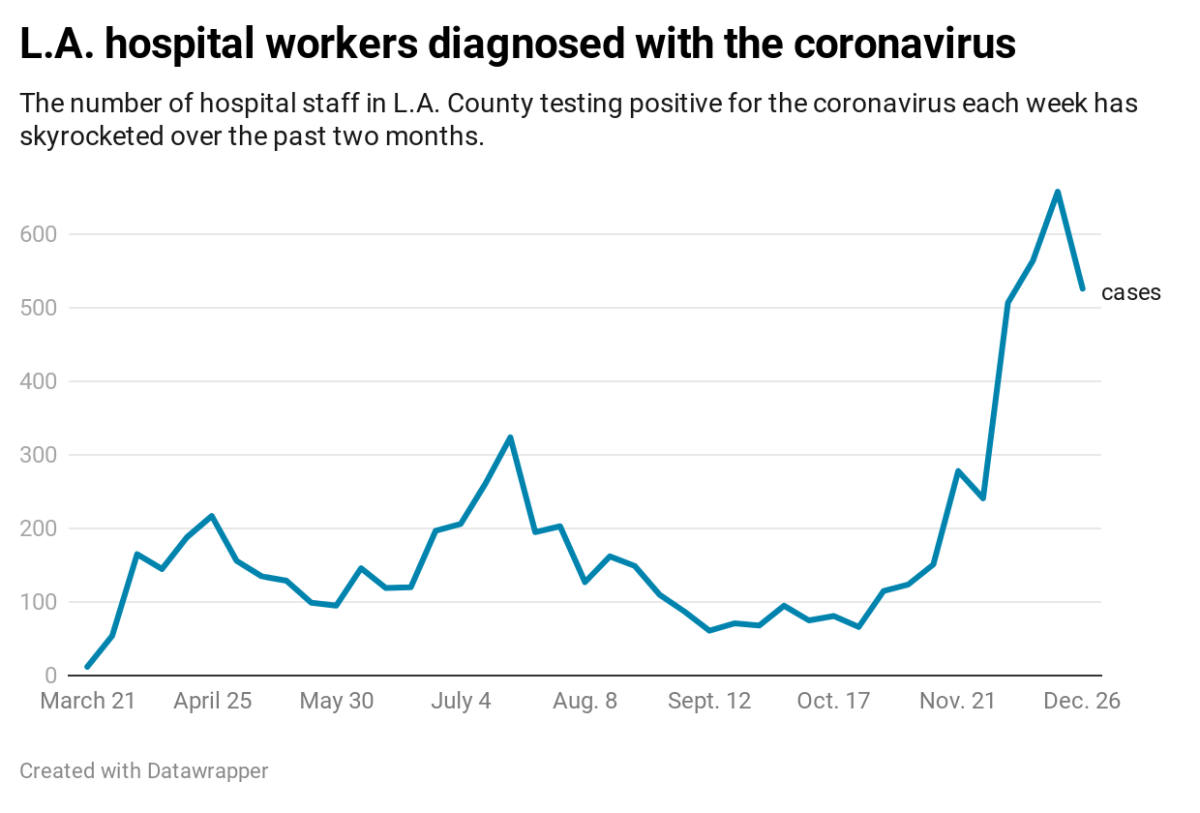
Infections among healthcare workers have swelled as overall cases have grown. In a single week in mid-December, as L.A. County reported more coronavirus infections than ever, 2,363 healthcare workers and first responders fell ill with COVID-19, compared with 360 two months prior.
Hospitals are where these problems compound. Nurses and doctors are stretched thin as COVID-19 patients overrun hospitals, and staff are out with the disease themselves, said UCLA emergency room nurse Marcia Santini.
“We have COVID that’s rampant and we have a very sick population — coupled with that we have a staffing crisis,” she said. “All of that combined is putting a real stress on these facilities.”
Santini became sick with COVID-19 last month, though she is not certain how she contracted the virus. She cared for COVID-19 patients before becoming ill, but her husband showed symptoms before her, suggesting he got it at work and then passed it on to her.
Her illness became so severe that she couldn’t breathe and was admitted to the hospital for days. Nearly three weeks later, she remains easily fatigued. “I’ve never gone through anything like this,” she said.
At Kaiser Permanente San Jose Medical Center, at least 43 staff members recently contracted the coronavirus, including one who died, part of an outbreak possibly linked to an employee who wore an inflatable holiday costume in the hospital to lift spirits.
In Fresno County, where only 11 ICU beds remained available Tuesday, a recent rash of healthcare workers falling ill or needing to stay home due to exposure to the virus has hampered hospitals’ ability to treat patients, said interim health officer Dr. Rais Vohra.
California registered more than 74,000 new coronavirus cases Monday — 11% higher than the previous record for a single day.
“We have hundreds of people who are out who could otherwise be working in our hospitals,” Vohra said. “There are so many cases that are happening, whether it’s a healthcare worker who’s sick or a relative who’s ill, that really affects our ability to deliver care because that person then has to take time off.”
Unlike in the spring, when a shortage of personal protective gear and ventilators was the most pressing issue, concerns during this latest surge have been largely centered around staffing. The U.S. Department of Defense is lending combat medics and nurses to assist hospitals across California.
L.A. County officials have redeployed nearly 800 clinic nurses to work in its public hospitals, while other local hospitals have recruited doctors and nurses from other departments to help out in the ICU, though with varying success.
“Quite frankly, you get comfortable in your field of knowledge, and when you’re put somewhere else, you’re a little bit of a fish out of water,” said Dr. Frank Candela, who is on the medical executive committee of West Hills Hospital. “People are spread thin. They’re persevering. They’re adapting, but it puts a big strain on the person doing it, as well as patient care.”
Many healthcare workers cited the emotional toll of seeing not just strangers severely ill, but their own colleagues hospitalized with the virus, or even killed by it. Candela said that Ernesto Ruelas, an environmental service worker at the hospital, died of COVID-19 this week. “He is deeply missed,” Candela said.
For the most part, staff who are falling sick with COVID-19 are believed to have caught it outside the hospital, he said. But that hasn’t always been the case.
Top LAFD brass are using free Lyft rides, Google Nest gear and home security systems to entice firefighters unwilling to get a COVID-19 vaccine.
In an unfortunate incident over the summer, COVID-19 infections were transmitted among staff who spent time together in the break room, often without masks and distancing, he said. That outbreak ultimately spread to patients too, he said.
Candela said the hospital has since begun to stagger breaks so people don’t eat lunch at the same time and now prohibits bringing in food to share with others. But he said he hopes his hospital’s experience shows the public that even small lapses can have devastating consequences.
“We sort of learned the lesson the hard way: that we can’t let our guard down,” he said.
This dark moment of the pandemic is brightened by ongoing vaccinations, healthcare workers say.
The first people vaccinated in California will receive their second dose this week, which offers 95% immunity to the coronavirus. With that protection, hospitals eventually won’t be so short-staffed, Mahajan said.
“Right now is the worst time because the vaccine hasn’t been out long enough,” he said. “But that’s going to be less and less of an issue as the days and weeks of January go by.”
Mahajan has warned his staff that the extreme surge will continue for at least five more weeks. L.A. County officials said this week that they expect the number of people hospitalized with COVID-19 to grow by at least 1,000 within the next two weeks, though only about 20 ICU beds are available.
“One of the things I’ve tried to tell our staff as we entered the Christmas holidays is that this is halftime,” Mahajan said. “I’ve asked them to pace themselves over the holidays — take some time for themselves and their families — because we have so much more we have to do.”
More to Read
Start your day right
Sign up for Essential California for news, features and recommendations from the L.A. Times and beyond in your inbox six days a week.
You may occasionally receive promotional content from the Los Angeles Times.










