HealthCare Partners seeks license to operate as managed-care plan
HealthCare Partners, the medical-group giant acquired last year by dialysis chain DaVita Inc. for $4.4 billion, is seeking a state license to operate as a managed-care plan after questions were raised about its compliance with California law.
The California Department of Managed Health Care has been looking into the nation’s largest operator of physician groups since last fall when a patient sued the Torrance company and accused it of acting like a health plan without the necessary Knox-Keene Act license. A spokeswoman for the managed-care agency said the allegations against HealthCare Partners “are still under review.”
The case is part of a wider debate about whether regulatory oversight is keeping pace with consolidation among doctors, hospitals and insurers and changes in medical payment sparked by the federal healthcare law. A state healthcare board is expected to discuss these matters Monday in Sacramento.
HealthCare Partners, which runs large medical groups in Southern California and four other states, had $2.4 billion in revenue in 2011 and serves about 750,000 patients, including more than 190,000 in Medicare Advantage plans. The combined company, called DaVita HealthCare Partners, is based in Denver.
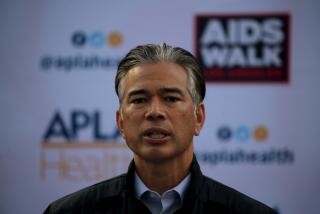
William Chin, executive medical director at HealthCare Partners, said the company is in full compliance with current law and its application for a limited health plan license is unrelated to the recent complaint.
Chin said the state license hasn’t been necessary before because the company contracted with licensed health plans to care for their patients, but new initiatives with Medicare require a different arrangement.
“We are in violation of no statute or law,” Chin said. The state “has reviewed these relationships and contracts for decades.”
State regulators require insurers and other “risk-bearing organizations” to hold adequate reserves to pay medical bills and to comply with patient protections.
California Senate President Pro Tem Darrell Steinberg (D-Sacramento) asked officials to address these concerns about licensing in November, records show.
In December, Brent Barnhart, director of the Department of Managed Health Care, responded in a letter that the agency “has been actively engaged in discussions with HealthCare Partners regarding its business model.”
Steinberg also asked whether the state had a conflict of interest because a HealthCare Partners executive and physician, Keith Wilson, serves as chairman of the agency’s Financial Standards Solvency Board. The board advises the agency on certain rules for health plans and medical providers.
“Dr. Wilson’s hand in advising the regulation of accountable-care organizations could be viewed as a contributing factor to a biased investigation,” Steinberg wrote in his Nov. 20 letter.
The board is scheduled to discuss this potential conflict of interest at its meeting Monday. Barnhart told Steinberg that he plans to “reconfigure the makeup of the board to include additional consumer representation” later this year.
A spokesman for Steinberg said the lawmaker is awaiting more information from the healthcare agency before commenting further.
The senator’s concerns stemmed from a lawsuit filed in September by Healthcare Partners patient Juan Carlos Jandres in Los Angeles County Superior Court. The suit alleges that the company engaged in unfair and fraudulent business practices. An additional plaintiff and former HealthCare Partners employee, Corey Hambrick, joined the suit last month.
Jandres sought care in 2010 for a growth in his mouth, according to his suit. He contends HealthCare Partners denied him access to appropriate hospital care because it was trying to avoid hospital claims it was responsible for paying. As a result, according to the suit, Jandres lost most of his jaw to cancer. Chin said the allegations of poor patient care are untrue.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.