Healthcare partnership pays big dividends
A rare alliance of healthcare rivals — a giant insurance company, a major hospital chain and a large doctors group — has managed to reduce healthcare costs through a radical new strategy: working together.
The collaboration among Blue Shield of California, Catholic Healthcare West and Hill Physicians Medical Group shaved more than $20 million in costs last year and prevented an insurance rate hike for public sector workers in Northern California.
The three partners cite evidence that the quality of care also improved: Hospital stays were shorter, readmissions dropped and doctors and nurses kept closer tabs on patients.
Relationships between these kinds of companies are typically adversarial, with doctors and hospitals trying to negotiate higher prices for their services as insurers strive to limit what they pay out.
But driven by a mutual interest to cut costs and to be more competitive, the three devised a strategy they believed would deliver medical care more efficiently.
Skeptics worry that the partnership and others like it will put cost-cutting ahead of patient care. Healthcare experts believe, however, that such experiments — including one being planned in Orange County — hold important lessons for an expected wave of similar “accountable care organizations” as part of the nation’s healthcare overhaul.
“The fact that they achieved substantial savings in the first year highlights the potential for the model,” said Dr. Elliott Fisher of the Dartmouth Institute for Health Policy and Clinical Practice in New Hampshire. “There are a lot of opportunities to achieve savings, even in the short term.”
The three partners began planning their experiment in early 2008 — well before President Obama and Congress opened a heated national debate over how best to control healthcare spending.
Their talks centered on 41,500 members of a Blue Shield HMO who were served by Hill Physicians, whose doctors are affiliated with Catholic Healthcare West, the state’s largest hospital chain.
All of the participants got their Blue Shield insurance through the California Public Employees’ Retirement System and lived in Sacramento, El Dorado and Placer counties.
Senior executives from the three healthcare companies said they had to overcome past quarrels to collaborate.
“Our staffs had a history of combating with each other through negotiations,” said John Wray, a senior vice president with Catholic Healthcare West. “We had to trust one another to make it happen. This was a very significant culture change between the organizations.”
The partners overhauled procedures for medical treatment and hospital care. They started by taking the extraordinary step of sharing closely guarded financial and medical information.
They discovered, for example, that a handful of elective procedures — including weight-control measures — were among the biggest cost drivers.
They took action to cut these costs. Overweight patients, for instance, were given an opportunity to enroll in a Hill Physicians weight-loss program in which a psychotherapist and dietitian teach how to manage food cravings and make healthier eating choices.
The efforts helped reduce the surgeries by 13% last year, the hospital system reported.
Emergencies were another target. When patients were taken to hospitals outside of Catholic Healthcare West, they were stabilized and then directed back to the hospital system for lower-cost “in-network” treatment. In all, 113 patients in the experiment went to emergency rooms outside the network last year. Of them, 85 were transferred back to Catholic Healthcare West hospitals once stabilized.
Medical centers and doctors also took aim at expensive repeat visits for hospital patients by paying greater attention to follow-up care. As part of the hospitals’ checkout procedures, nurses reviewed patients’ post-hospital instructions and then asked them to repeat it all back. The providers also made sure patients had made appointments with doctors before going home.
As a result, hospital stays overall were shortened and the numbers of patients who had to be readmitted dropped by 15% in 2010, the providers said. Both results, they said, were signs of improved care: Spending less time in the hospital meant less chance of getting infections, while fewer readmissions meant patients remained healthier after surgery.
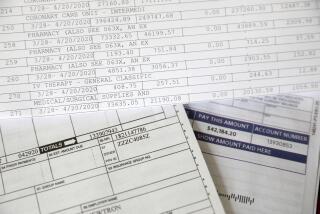
Of the $20 million in savings, Blue Shield recouped $15.5 million for a pledge it had made to CalPERS not to increase insurance rates for the 41,500 people in the experiment. The remaining $5 million was divvied up among the three partners. They also had agreed to share the risk if the experiment didn’t pay off.
Blue Shield executives believe the rate cut helped attract about 1,000 new policyholders last year and gave the company a competitive edge as it vied for a new CalPERS contract. Blue Shield covers more than 400,000 CalPERS members, about one-third of those who get health insurance through the giant state pension fund.
“Clearly it was worth our while,” said Juan Davila, Blue Shield’s top executive who oversees provider contracting. “Our biggest client is happy with us.”
Some healthcare advocates question whether patient health will suffer as Blue Shield and its partners look for additional cost savings. Could procedures or tests be denied because they are too expensive, they ask.
“You want to make sure that people have access to the care they need,” said Anthony Wright, executive director of the consumer group Health Access California. “That’s part of the balancing act.”
The experiment’s three partners insist that healthcare quality is as important as saving money.
CalPERS, meanwhile, said it is pleased to see improvements on both fronts, even though most of the savings in Northern California went unnoticed by individuals because the money was shared among the agency’s entire statewide membership.
Blue Shield is joining with hospitals and medical groups for similar alliances in San Francisco, Modesto and Orange County. The insurer and St. Joseph Health System in Orange are gearing up to launch a collaboration in January for 30,000 Blue Shield HMO members. About one-quarter of them belong to CalPERS.
“We firmly think this is the right way to go,” said Ann Boynton, a CalPERS benefits executive. The cost-cutting strategy, she said, “will boost care for our members and moderate the long-term increases in cost.”
More to Read
Sign up for our L.A. Times Plants newsletter
At the start of each month, get a roundup of upcoming plant-related activities and events in Southern California, along with links to tips and articles you may have missed.
You may occasionally receive promotional content from the Los Angeles Times.