Q&A: Will the Anthem-Cigna deal cost you money?

Anthem is buying rival Cigna in a $54-billion deal.
Anthem Inc., California’s largest for-profit health insurer, has agreed to acquire rival Cigna Corp. for $54 billion.
The planned merger is the latest in a string of health insurance deals announced in the last few weeks. Aetna Inc. reached a $37-billion deal for Humana Inc. this month. And Woodland Hills insurer Health Net Inc. agreed to be acquired by Medicaid insurer Centene Corp. for $6.8 billion.
Here’s what you need to know about consolidation in the healthcare industry:
What does the Anthem-Cigna deal do?
It would create the largest U.S. health insurer by enrollment. The combined company would generate about $115 billion in annual revenue and have 53 million members.
What’s the effect on consumers?
Some lawmakers, employers and consumer groups are worried that consolidation will drive up premiums at a time when the cost of coverage is already high for many families.
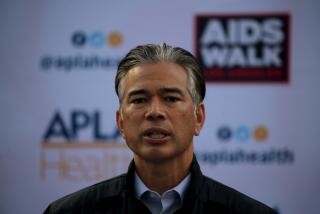
Dave Jones, California’s insurance commissioner, said he doubts there will be any significant benefits from this round of mergers.
Friday, he declined to comment specifically on the Anthem deal before reviewing it further. But generally, he said, increased consolidation has resulted in less competition and higher pricing.
“I do have concerns about the merger activity in the health insurance market,” Jones said.
Proponents say a larger health insurer could persuade hospitals, physician groups and pharmaceutical companies to offer lower prices based on the high membership numbers, and that those savings could be passed down to policyholders.
The effect on individual consumers will also vary by region. In some areas, there may be local health plans that offer another alternative.
Why are these deals happening now?
The Affordable Care Act imposes limits on health insurers’ profits, so these companies view consolidation as the best way to lower costs and take advantage of rising revenues. The insurers also see a combination as a way to capitalize on the increasing privatization of Medicare and Medicaid.
When will the merger close?
Anthem expects the deal to close in the second half of 2016. But health-policy experts expect a lengthy review by antitrust authorities and other state regulators that could slow down the process.
For more business news, follow @smasunaga.
ALSO:
Using a health savings account for medical costs — and retirement
Aetna’s 21% rate hike amounts to ‘price gouging,’ California regulator says
Healthcare law helps sickest Americans — depending on their state
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.