Amid ‘viral tsunami,’ Army Corps of Engineers will aid L.A. hospitals facing oxygen problems

It was the first day of a fresh year, and yet, across much of California, the numbing realities we had longed to put behind us — hospitals at capacity, mounting death tolls, and massive, maskless gatherings — have followed us into 2021.
On Friday, the number of Californians who have died from complications of COVID-19 passed 26,000 — roughly the same number of Californians who, in a recent year, died of complications of the flu, diabetes, hypertension and liver disease combined.
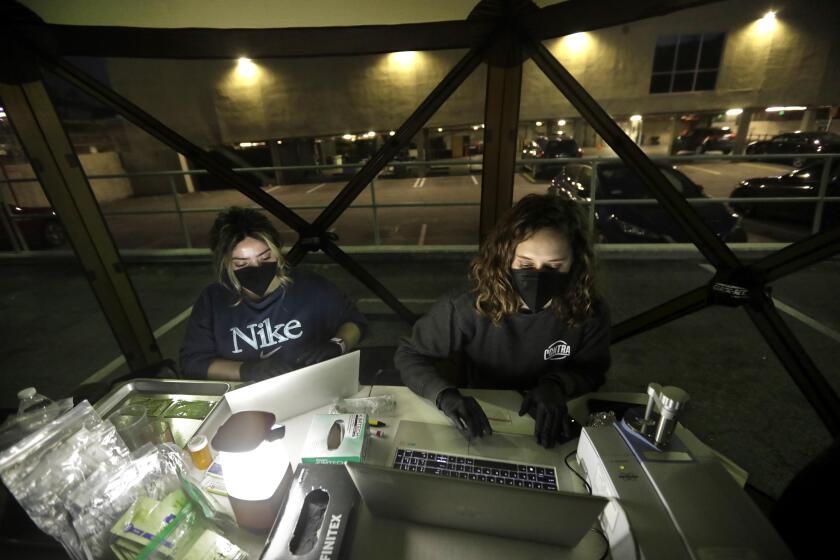
In L.A. County, where hospitals have gotten so backed up that patients have had to wait outside in ambulances for up to eight hours, hope for some respite finally arrived Friday: The Army Corps of Engineers was planning to send specialized crews to the region to update oxygen-delivery systems at a handful of aging hospitals.
Days earlier, several hospitals declared internal disasters and temporarily turned away all ambulance traffic because their internal oxygen systems began to buckle beneath the high demand of air flow needed by patients whose lungs had been ravaged by the coronavirus.
As emergency rooms and intensive care units across the county remain overwhelmed by patients with the respiratory disease, hospitals continue to buckle under the dangerous ripple effects that have impacted nearly all aspects of medical care.
With 700 nurses from primary care clinics diverted to hospitals and other critical needs, county officials have been forced to temporarily shut five public primary care clinics across the county and reduce hours at most of the others, which provide children with immunizations and where people with chronic diseases have their medications managed.
“We have kept a skeleton crew to continue to work in our outpatient clinics,” said Dr. Christina Ghaly, the L.A. County director of health services. “But overall, our capacity for outpatient services is much less than it is in routine times.”
This means that patients with chronic illnesses will be at greater risk of needing to go to the emergency room if they become more seriously ill because of the lack of outpatient care.
And it means, too, that hundreds of procedures and surgeries have been put on pause.
For Matt Howard — a 44-year-old high school teacher who was scheduled to have kidney transplant surgery at Cedars-Sinai on Jan. 15 — it meant receiving a disappointing phone call on a recent afternoon.
“We’re sorry,” the voice on the other line said. “There are no ICU beds available, so we have to postpone the surgery.”
When he told his wife, she broke down in sobs. His two daughters, 20 and 22, were devastated as well. But Howard, who lives in Lakewood, said he takes some comfort in knowing that his donor — his older sister — isn’t going anywhere. It would have been a much worse situation, he said, if he’d been scheduled to receive a new kidney from a recently deceased donor.
Hospitals are doing the best they can in impossible circumstances, he said, and he places no blame on them for the cancellation. Still, he said, he’s eager for the transplant. The last time he had his kidneys checked, doctors told him they were functioning at 3%, said Howard, who undergoes nine-hour dialysis treatments at home every night.
“It’s a waiting game,” he said, noting that he doesn’t yet have a new surgery date scheduled.
The situation at many medical facilities across the Southland remains dire.
Paramedics now regularly decide not to transport lower-risk patients to overcrowded hospitals, hoping to free up space for those most in need, which has forced people who might otherwise go to the emergency room to look elsewhere for care.
Hospitals are scrambling to find sufficient staff and, at times, emergency medical technicians have been called into work at hospitals. Meanwhile, older hospitals are being reconfigured to house far more patients than they ever anticipated holding, leading to the oxygen issues.
Dr. Christina Ghaly, L.A. County health services director, said that the demand is so great for a high flow of oxygen and the buildings pipes are so old, they can’t maintain sufficient pressure and, at times, started to freeze. In a scramble, Ghaly said, some hospitals were forced to move patients to lower floors, because it’s easier to deliver oxygen there without needing pressure to push it up to higher floors.
Another oxygen-related problem — the chronic shortage of portable tanks — has also hampered hospitals abilities in recent days, county officials said. To discharge recovering patients as quickly as possible and free up space for other, sicker patients, hospitals often send patients home with oxygen tanks.
The team of design and construction experts from the Corps will evaluate six hospitals — Adventist Health White Memorial in Boyle Heights, Beverly Community Hospital in Montebello, Emanate Health Queen of the Valley Hospital in West Covina, Lakewood Regional Medical Center, Mission Community Hospital in Panorama City and PIH Health Hospital in Downey — and then oversee upgrades where they’re deemed necessary.
Mark Ghilarducci, director of the California Governor’s Office of Emergency Services, said in a statement that the upgrades will “improve the ability to deliver life sustaining medical care to those who need it.”
The assessments are scheduled to begin as soon as Saturday, state officials said.
L.A. County has been forced to temporarily shut down five public primary care clinics to help staff hospitals amid a deadly surge in coronavirus cases.
The basic problem is that patients, suffocating from their inflamed lungs, are demanding such a high flow of oxygen to the extent that some hospitals cannot meet the demand with existing infrastructure.
“Running low of oxygen and oxygen tanks is an issue,” said Cathy Chidester, director of the L.A. County Emergency Medical Services Agency.
And L.A. County Public Health Director Barbara Ferrer has said she expects these trends to continue for several weeks.
“We’re experiencing extreme conditions in L.A. County,” she said. “Our hospitals continue to be overwhelmed. As more and more people are rushed to hospitals, the tragic fact is that hundreds more people will die every week from COVID-19. These trends, unfortunately, will continue into January.”
And yet, there was one small bit of hopeful news released on New Year’s Day. For the first time in 50 days, the net number of people hospitalized in L.A. County for COVID-19 decreased — although only by one. Still, it broke the 32-day consecutive daily streak of record-breaking COVID-19 hospitalizations in L.A. County.
On New Year’s Eve, there were 7,627 COVID-19 patients hospitalized in L.A. County, down from 7,628 the day before, according to data released Friday.
The slower increase in daily patients is a sign that the stay-at-home order in place in Southern California for nearly four weeks is having an impact.
“There’s no question in my mind that had we not had the stay-at-home order, the situation would be far more dire than it is now,” said Dr. Robert Kim-Farley, medical epidemiologist and infectious diseases expert at the UCLA Fielding School of Public Health, who described the current situation as a “viral tsunami.”
“However, I think the magnitude of the numbers show that in the face of the stay-at-home order, many people are choosing to ignore it,” he said, adding that any slight easing in new hospitalizations will likely be reversed soon because of how many people traveled during Christmas and New Year’s.
For Howard, the teacher awaiting a transplant, it is deeply frustrating to see people refusing to wear masks or going out to New Year’s Eve parties.
“It’s disappointing,” he said.
When Howard was diagnosed with IgA nephropathy four years ago, his kidney function was at 30%. When it dropped below 10% last year, he started doing dialysis via a catheter in his stomach lining. Even with the treatments, he said, he constantly feels exhausted.
A high school football coach, he said he yearns to return to the level of energy and drive he once felt. He dreams about riding his bike to work again and, when the pandemic is behind us, one day traveling with his wife.
For his sister, Gail Houseweart, a labor-and-delivery nurse in Colorado, news of the delayed surgery was heartbreaking.
After scores of blood tests — involving 33 vials in all, she recalls — and undergoing a full day of tests, including a mammogram and a chest X-ray, she finally got the green light about a month ago: She was a match, and they were all set. She was elated. When people told her she was a hero, she responded that, no, in fact, she felt selfish. She needed her little brother.
“I want him around for me and his kids and his wife,” she said.
She bought a plane ticket to Los Angeles and booked an Airbnb for after the procedure, but then she got the call about the cancellation. She went it a funk for a couple of weeks, she said, but she is trying to focus on the future.
“2021 is our year,” she says, pausing. “I guess, I hope.”
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.