ICU availability in Southern California at 0%, and it’s going to get worse, officials warn

The availability of intensive care unit beds throughout Southern California hit 0% Thursday, and officials warned that conditions in hospitals are expected to erode further if the coronavirus continues to spread unchecked.
With ICUs filled, hospitals will step up measures to ensure the sickest patients still get the highest levels of care possible. That often means moving some patients who would typically be in the intensive care unit to other areas of the hospital, such as a recovery area, or keeping them in the emergency room for longer than normal.
The patients are still getting intensive care, and that strategy can work to a point. But eventually, there may be too many critically ill patients for the limited numbers of ICU doctors and nurses available, leading to greater chances of patients not getting the specialized care they need. And that can lead to increases in mortality.
ICU availability in Southern California at 0%, and the crisis is expected to get worse, officials warn.
Once ICU beds are full, hospitals go into surge mode, which can accommodate 20% over usual capacity. Officials have also been training medical personnel who work elsewhere in hospitals to allow them to work in ICUs, and seeking nurses from outside the United States.
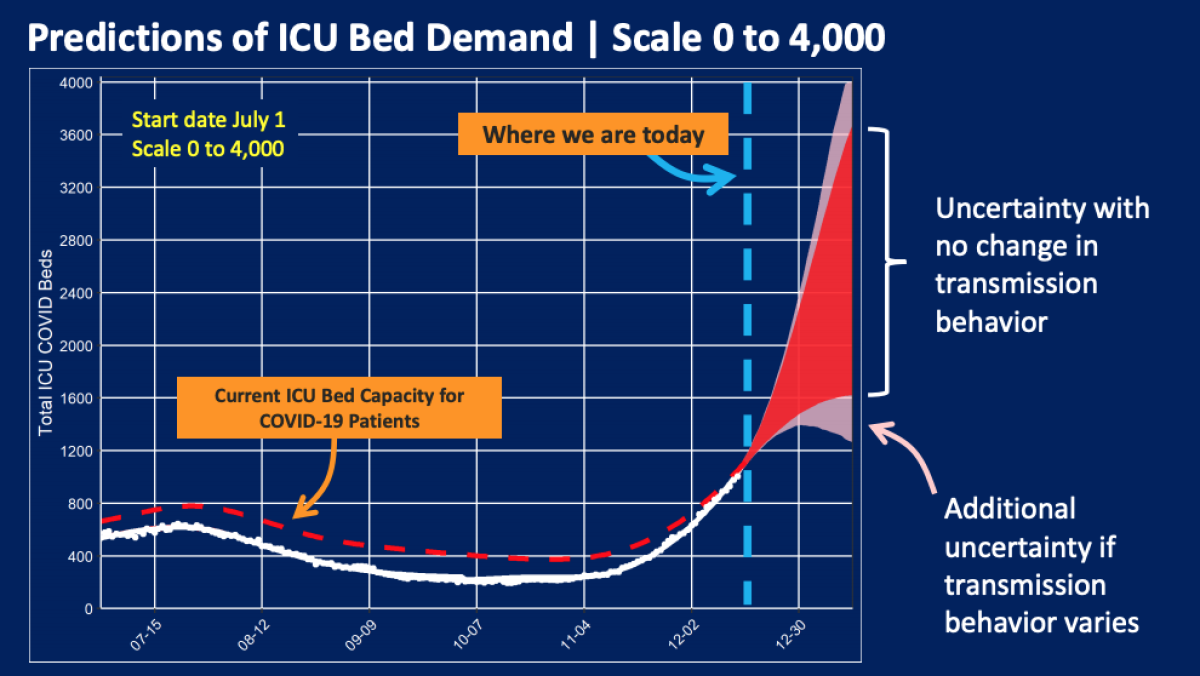
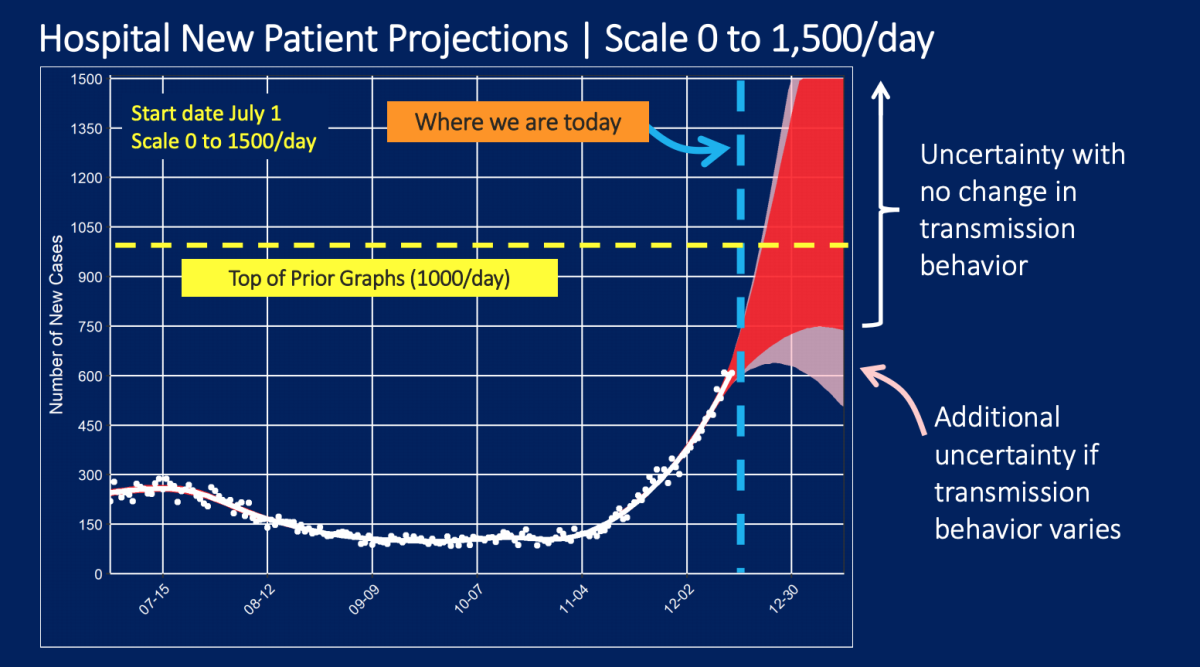
But the forecasted size of the surge of severely ill COVID-19 patients needing hospitalization in the coming weeks is now so large, it blew past projections issued just a few weeks ago. Officials were forced to redraw their charts to accommodate the enormous surges in projected ICU bed demand.
There are now more than 1,000 people with COVID-19 in L.A. County’s intensive care units, quadruple the number from Nov. 1. Forecasts say that by early January, there could be 1,600 to 3,600 COVID-19 patients in need of ICU beds if virus transmission trends remain the same.
There are only 2,500 licensed ICU beds in L.A. County.
“There are simply not enough trained staff to care for the volume of patients that are projected to come and need care,” Dr. Christina Ghaly, the county’s director of health services, said. “Our hospitals are under siege, and our model shows no end in sight.”
About 600 new patients with COVID-19 are now being admitted to hospitals daily in L.A. County, and officials say that could rise to 750 to 1,350 a day by New Year’s Eve.
“If the numbers continue to increase the way they have, I am afraid that we may run out of capacity within our hospitals,” said Dr. Denise Whitfield, associate medical director with the L.A. County emergency medical services agency and an emergency room physician at Harbor-UCLA Medical Center. “And the level of care that every resident in Los Angeles County deserves may be threatened just by the fact that we are overwhelmed.”
Though officials have noted that the number of available ICU beds changes constantly as new patients are admitted, stabilized or die, the number of unoccupied beds in California’s most populous region has steadily eroded as hospitals have been flooded by unprecedented numbers of COVID-19 patients.
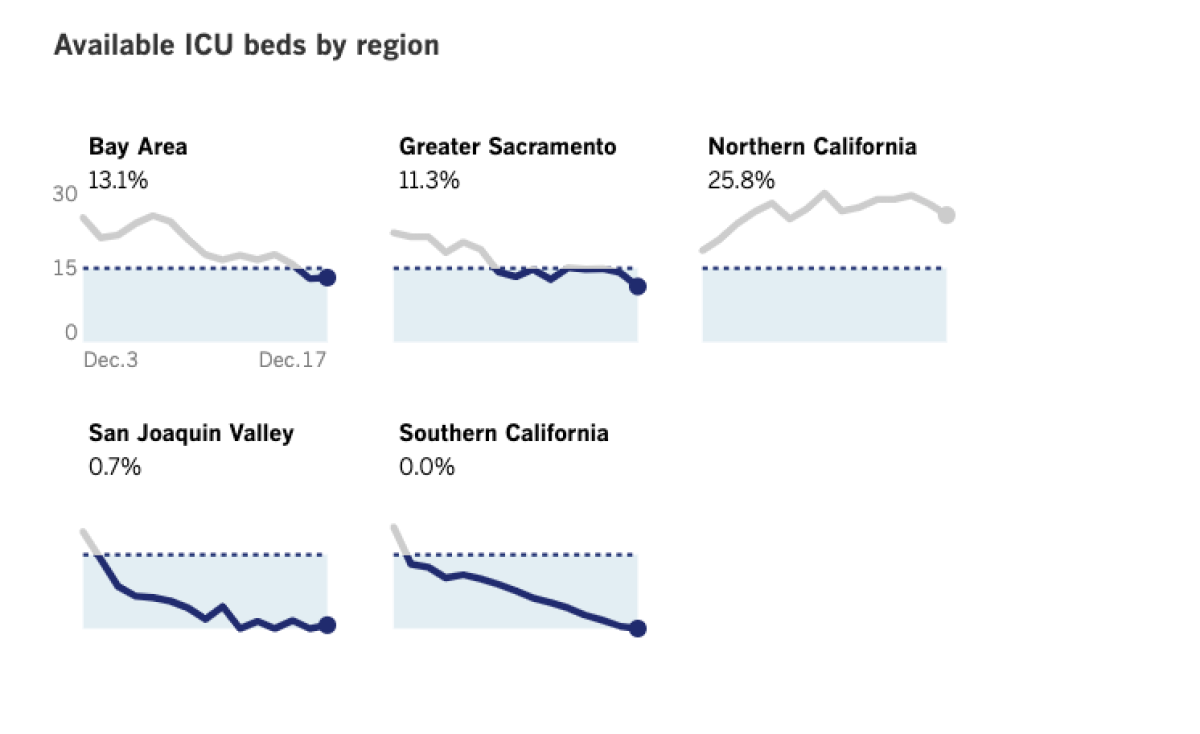
ICU availability throughout Southern California — which the state defines as Imperial, Inyo, Los Angeles, Mono, Orange, Riverside, San Bernardino, San Diego, San Luis Obispo, Santa Barbara and Ventura counties — had been a scant 0.5% Wednesday before falling to zero Thursday.
The San Joaquin Valley — which has hit 0% availability in its ICUs a few times in recent days, most recently Wednesday — saw that number tick up slightly Thursday, to a still-perilous 0.7%.
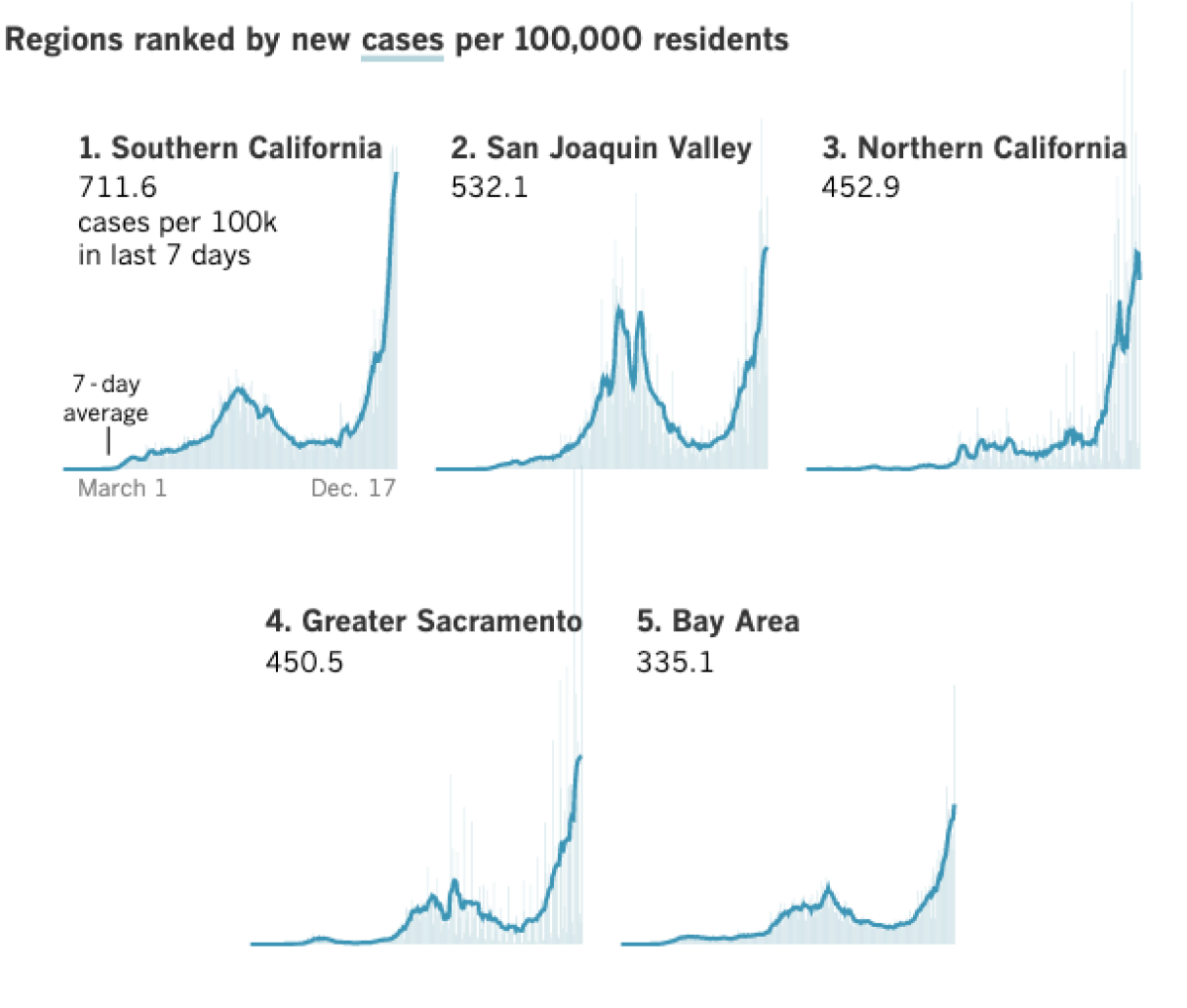
Both regions in the southern half of the state have the worst rates of new coronavirus cases on a per capita basis. In the last week, Southern California is reporting 712 coronavirus cases per 100,000 residents, and the San Joaquin Valley, 532 cases per 100,000 residents.
By contrast, the greater Sacramento area is reporting 451 coronavirus cases per 100,000 residents, and the Bay Area, 335 cases per 100,000 residents, over the same time period.
Officials in L.A. County believe hospitals will be hit by a wave of patients in the coming weeks much larger than previously expected.
California is now opening temporary field hospitals to help with overflow patients. The field hospitals will care for non-ICU patients in places such as Porterville, Sacramento, Imperial and Orange County; other facilities are on standby status in Riverside, Richmond, Fresno, San Diego and San Francisco.
Public health officials are anxiously tracking the capacity of intensive care units as coronavirus case numbers surge. Why is that metric important?
The number of people hospitalized in California for COVID-19 has broken records for 19 consecutive days. On Wednesday, the most recent data available, 15,431 people across the state were in hospitals with coronavirus infections — more than six times more than the number on Halloween.
The virus was touching all corners of the region. Los Angeles Mayor Eric Garcetti said Thursday that his 9-year-old daughter, Maya, had tested positive. Both Garcetti and his wife tested negative, he said.
Garcetti said he doesn’t know how his daughter was infected. “We haven’t mixed households,” he said. “There’s no behavior that she is engaged in that doesn’t adhere strictly to the protocols of our health officials.”
To contain the spread of COVID-19, parks, restaurants and stores are slowly reopening.
Because of the lagging nature of the novel coronavirus, it can take two to three weeks for spikes in cases to trigger a corresponding increase in hospitalizations. When that happens, though, the consequences can be sudden and severe. State officials have previously estimated that 12% of newly diagnosed coronavirus cases are likely to require hospitalization, with 12% of those eventually ending up in the ICU.
That means the most recent record-high hospitalizations do not account for the sky-high numbers of new infections, a chilling prospect for the state’s stretched-thin hospitals and healthcare workers. State officials this week said they expect hospitalizations to worsen particularly in the lead-up to Christmas and New Year’s Day.
Hospitals in L.A. County are desperately trying to free up beds by discharging recovering patients as quickly as possible, but there is only so much longer that hospitals can stretch their staff to meet the demand until the quality of patient care starts to worsen.
“Many hospitals have already broken nurse staffing ratios, and their staff are not necessarily getting either the breaks or rest that they’re supposed to be getting,” Ghaly said.
Last weekend, Whitfield said, Harbor-UCLA was able to manage its COVID patients, but crowding meant that some patients needed to stay in the emergency department when they should have been transferred elsewhere in the hospital.
“What that means is that when a patient needs to be admitted to the hospital, requiring either an ICU or an inpatient bed, that we just don’t have the staffing or the actual bed space to care for them,” Whitfield said.
A backed-up emergency room then makes it harder for emergency physicians and nurses to take care of patients with other emergencies, including strokes, heart attacks and trauma.
Whitfield said she’s been an emergency room doctor for a decade, but the past weekend was the first time she felt the overcrowding situation “has actually threatened the level of care that we can provide for our patients.”
“And so looking at ... how these numbers are increasing throughout the county, it’s really, really quite frightening to me,” Whitfield said.
The surge in coronavirus cases continues to set records. For the first time, a Los Angeles Times county-by-county tally found more than 50,000 new coronavirus cases and nearly 400 deaths in California reported in a single day. A Times survey Wednesday night found 51,724 new coronavirus cases reported, shattering the state’s previous record, set Monday, when 42,088 cases were reported.
The latest maps and charts on the spread of COVID-19 in Los Angeles County, including cases, deaths, closures and restrictions.
The Times tally also found 393 COVID-19 deaths Wednesday across California, breaking the record set Tuesday, when 295 deaths were recorded.
On Thursday, 51,209 coronavirus cases were reported statewide — the second-highest single-day tally. There were 288 deaths reported Thursday, the third-highest single-day tally.
Cumulatively, California has now reported 1.7 million coronavirus cases and more than 22,000 COVID-19 deaths.
The state is now recording an average of 220 COVID-19 deaths a day over a weekly period, and about 38,000 daily cases — both records, and both quadruple the numbers from mid-November.
San Francisco issued a travel order effective Friday requiring anyone visiting, moving or returning to the city from outside the Bay Area to quarantine for 10 days.
Dr. Grant Colfax, the city’s public health director, announced the 10-day quarantine travel order amid a ‘staggering’ increase in coronavirus cases.
The mandatory order takes effect at 12:01 a.m. Friday. Violating the order is a misdemeanor. Medical workers, first responders and essential workers are exempt.
San Francisco’s travel order follows one issued by Santa Clara County in late November requiring people to quarantine for 14 days after returning from travel of more than 150 miles.
Times staff writers Maura Dolan, Sean Greene and Dakota Smith contributed to this report.
More to Read
Start your day right
Sign up for Essential California for news, features and recommendations from the L.A. Times and beyond in your inbox six days a week.
You may occasionally receive promotional content from the Los Angeles Times.















