Doctors call pay method flawed
- Share via
Insurance companies often fail to properly reimburse doctors, needlessly adding more than $200 billion a year to the nation’s healthcare tab, the American Medical Assn. said Monday.
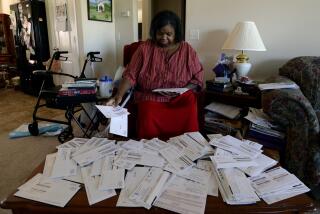
An analysis of 3 million medical claims over a six-month period beginning in October also found that doctors in the U.S. spend 14% of the fees they receive from insurers and Medicare on the process of collecting those fees, the AMA said in a report issued at its annual meeting in Chicago.
The analysis sized up insurers and Medicare on how often they paid on time, how often they denied claims and how often they paid at the contracted rate and other measures.
Medicare outperformed commercial insurers in many areas, and some insurers paid physicians’ bills better than others.
For example UnitedHealthcare, whose parent owns California’s PacifiCare, paid physicians the contracted fee 62% of the time. By comparison, Aetna Inc. paid the contracted fee 71% of the time and Medicare paid the set fee 98% of the time.
The report, part of a campaign to reduce inefficiencies in claims payments, was the AMA’s first effort to quantify the red tape and hassle that have sent many physicians into cash-only “concierge” practices or early retirement.
Improving the processing of medical claims could reduce overall costs to patients, physicians, insurers and others, the report said.
“The goal of the AMA campaign is to hold health insurance companies accountable for making claims processing more cost-effective and transparent and to educate and empower physicians so they are no longer at the mercy of a chaotic payment system that takes countless hours away from patient care,” said AMA board member Dr. William A. Dolan.
A spokeswoman for America’s Health Insurance Plans, a Washington trade group for insurers, said the industry was working to expand electronic claims payment processes and make other changes in an effort to pay more promptly and accurately.
But the spokeswoman, Susan Pisano, said physicians shared some of the blame.
“In order for claims to be processed quickly and correctly, there are two parties that have to do their jobs,” Pisano said.
UnitedHealthcare spokesman Gregory Thompson said, “Data show there is often a significant lag time between when services are provided and physician claims are submitted.” Peter Lee of the Pacific Business Group on Health, a San Francisco-based coalition that represents large employers, said the report “lays down the gauntlet not only for health plans but also for elected officials to make sure healthcare reform creates a system that puts patients first and provides coverage rather than builds inefficiencies and waste that we have far too often.”
“Savings on administrative waste is low-hanging fruit, and the cost of extra paperwork is actually part of the reason we have millions of uninsured,” Lee said.
One reason cited for delays: when insurers ask doctors to resubmit claims or provide additional information before a claim can be paid. There was wide variation among insurers and Medicare on how long it took them to tell a physician that additional information was needed. Coventry Health Care, an insurer doing business predominantly in the South, had the fastest turnaround at five days. Humana Inc. was slowest, at 22 days. Cigna Corp. was next at 20 days, followed by Woodland Hills-based Health Net Inc. at 17 days.
The percentage of outright denials of claims varied by insurer, the report said, ranging from 3% (United and Coventry) to 7% (Medicare and Aetna). The reasons for denials include patients’ preexisting conditions, deductibles not being met, expenses incurred prior to coverage and expenses incurred after coverage ended.
Some physicians and healthcare experts pointed to the banking industry as a model. The industry has reduced transaction costs by having competing financial institutions use uniform documents and standard procedures. Some banks have opened healthcare franchises, helping hospitals and physician groups automate their claims collection processes. The AMA is pushing for the insurance industry to follow banking’s lead.
“Eliminating the inefficiencies of the billing and collection process would produce significant savings that could be better used to enhance patient care and help reduce overall healthcare costs,” the AMA’s Dolan said.
--
--
The Associated Press was used in compiling this report.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.