Big Increase in Venereal Warts Worries Doctors
- Share via
Jennifer had been expecting the news from her doctor, but she couldn’t help feeling embarrassed.
The 26-year-old data manager had been dating John when she learned he was infected with human papilloma virus or HPV, a highly contagious virus that causes venereal warts in both men and women.
Soon after meeting him, Jennifer’s Pap test was positive and a biopsy confirmed that her cervix was showing precancerous changes, both indications that she too had the virus.
Jennifer and John are just two of more than 1 million people in the United States who will be treated for venereal warts this year, according to the federal Centers for Disease Control in Atlanta.
Though venereal warts have been around for at least 2,000 years, since the days of the Greeks and Romans, only recently have physicians been sounding the alarm about this sexually transmitted disease and reporting cases in record numbers. There is mounting evidence suggesting that certain strains of HPV are linked to cancerous and precancerous changes of the cervix and genitals, researchers say.
Treatment Cuts Risk
“Of the 8,000 women who’ll die of genital cancer this year, we’ll find HPV in at least 7,000,” said Dr. Richard Reid, director of an obstetric-gynecologic research clinic at Detroit’s Sinai Hospital and a genital warts specialist. “HPV is probably the thing that sets up the changes that can lead to cancer.”
But those who have the virus needn’t be overly concerned, he emphasized. Once genital warts are detected and treated, “the chances of an individual coming to harm from this disease are low.”
Only a few strains of the nearly 50 known varieties of HPV have the potential to transform normal cells into malignant cells, researchers believe.
As with most venereal diseases, both partners should be treated to avoid reinfection. (Studies show that 50% to 80% of males contract venereal warts from their partners.)
Difficulties in Detection
Removal of the warts using a carbon dioxide laser and the application of anti-viral creams are often recommended. Other traditional treatments include chemicals, burning, freezing and surgical removal.
The problem remains detection. HPV can show up immediately after infection or lie dormant for years, say researchers. Some patients experience a rash, burning itch or cauliflower-like growth.
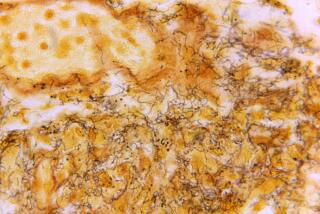
Doctors say small round bumps are sometimes visible on both the male and female sex organs, but most venereal warts cannot be seen by the naked eye. A Pap smear is the only certain way to confirm the presence of HPV, they note.
It’s a baffling virus and “the most dangerous venereal disease around,” according to Reid. “No two women get the exact same symptoms. It’s as individual as a fingerprint.”
Reid’s studies indicate that venereal warts are “several times more common” than herpes, gonorrhea or even chlamydia, until recently considered the No. 1 sexually transmitted disease in the U.S.
Still other research suggests that 5% of all women in the U.S. are infected, and a new study by doctors at the University of Washington found that 15% to 20% of women attending clinics for sexually transmitted diseases showed evidence of the virus.
Reports Not Required
But such statistics aren’t conclusive, said Dr. Katherine Stone at the Centers for Disease Control, because genital warts are not a reportable venereal disease. “Nobody was even looking for it five years ago,” she noted.
“It’s unbelievable how much of it we’re seeing,” said Dr. James Gordon, a gynecologist with the Women’s Medical Group of Santa Monica. In the last three years, he noted, the clinic’s caseload of new patients has jumped from two to 20 to 25 patients.
“It’s a huge problem that only doctors, patients and their partners know about,” concurred Dr. Richard Nalick, a gynecologic oncologist at Good Samaritan Hospital in Los Angeles who sees between 40 and 60 new cases a month. “There’s a whole sexually active population out there that doesn’t know anything about this.”
Yet physicians nationwide are demonstrating a new awareness of HPV. A survey of private doctors by the American College of Obstetricians and Gynecologists revealed a 459% increase in the number of patients seeking treatment for genital warts between 1966 and 1981.
Despite the growing attention, some experts believe the virus isn’t always detected. Unless it is picked up on a Pap smear or a physician uses a vinegar wash and colposcope to see the often tiny warts, chances are they will go untreated for years.
Higher-Risk Factors
At higher risk of infection, researchers say, are women who began intercourse at a young age, those who have had several pregnancies close together, those who have had multiple sexual partners and those who smoke cigarettes or take birth-control pills.
Also puzzling to researchers is why venereal warts appear to be getting bigger, more difficult to cure and more prevalent among young people.
According to Reid, 80% of venereal warts respond to treatment rapidly and easily. The carbon dioxide laser and anti-viral creams have done much to advance treatment of the warts, he added.
Injections of interferon--a natural virus-fighting protein--directly into the warts have shown limited promise as well, CDC’s Stone noted, although the treatment is expensive and can have some side effects, including flulike symptoms.
For difficult cases, hours of laser surgery and follow-up treatments may be necessary, Nalick said.
Doctors recommend that women in the high-risk category and those already diagnosed with venereal warts have Pap tests twice a year. Using a condom is another good preventive measure, they say, but it is not fail-safe.