Scientists Find New Way to Foil Staph Bacteria
- Share via
A revolutionary way to combat deadly antibiotic-resistant “superbugs” has been developed by researchers at UC Davis, perhaps paving the way for a new class of drugs to supplement antibiotics.
Rather than killing the bacteria, the researchers have made an end-run around the ability of bacteria to resist antibiotics--by attacking the mechanism through which they release toxins. It is these toxins, rather than the bacterial infection itself, that destroy tissues and impair vital organs, leading to serious illness and even death.
Working with the bacterium Staphylococcus aureus, which infects as many as 500,000 hospitalized Americans a year, the researchers have identified a key protein that enables the microorganism to release its toxins. Immunizing mice with this protein protects them from the lethal effects of a staph infection, the team reports today in the journal Science.
And because the treatment does not kill the bacterium, as antibiotics do, it is unlikely that the bacterium will be able to develop resistance to it.
“This opens a whole new strategy for treating or preventing one of the most serious hospital infections we contend with,” said infectious disease specialist Julie Gerberding of UC San Francisco.
Other bacteria, furthermore, almost certainly use an identical or similar mechanism for releasing their toxins, said Dr. Naomi Balaban of UC Davis, so this approach might work across a broad spectrum of infections.
“The implications are pretty enormous,” said Dr. Scott Harkonen of InterMune Pharmaceuticals Inc. in Palo Alto. “We need some breakthrough approaches to controlling these infections.”
Physicians have been in a life-and-death race with bacteria since penicillin was first used during World War II. As soon as researchers introduce a new antibiotic, bacteria begin developing resistance to it. Often, the useful life of an antibiotic may be as little as 10 years.
S. aureus is a particular problem, both because it can be so deadly and because it is common in hospitals. In recent years, physicians have found several strains of S. aureus that are resistant to all drugs except a powerful antibiotic called vancomycin.
Last year, they began to see infections that were resistant even to vancomycin, leaving them virtually helpless in treating patients. Even though more powerful drugs than vancomycin are in development, it appears that the mutational ability of the bacterium may be outrunning the innovations of chemists.
Balaban’s team has taken a completely different approach to controlling the infections.
Several years ago, while working in the lab of microbiologist Richard Novick at the New York University School of Medicine, Balaban discovered a protein called RAP. Each S. aureus bacterium secretes a small amount of RAP continuously and has receptors on its surface that measure the amount of RAP in its environment.
As the bacteria proliferate, the amount of RAP increases. Once a critical concentration of RAP is reached, indicating that the bacteria are becoming crowded, the protein triggers the release of toxins, which destroy tissue and make more room for the expanding bacterial colony.
Balaban reasoned that removing RAP from the bacteria’s environment would prevent toxin release. “If you take this molecule from the bacteria, they always think they are in bliss,” she said. “And if they are in bliss, they don’t have to release toxins and cause disease.”
She confirmed her suspicions by comparing cows that had had staph infections with cows that had not. The healthy cows had naturally occurring antibodies against RAP, while those that were infected had none.
She and colleagues at Davis, the University of Maryland and Panorama Research Inc. in Mountain View, Calif., then immunized mice with RAP, stimulating a response that prevented the protein from binding to the receptors. The mice were subsequently injected with a virulent strain of S. aureus that produces lesions on the skin called cellulitis. Seventy percent of the mice developed no lesions, and the remainder had lesions that were much smaller than normal.
The team also studied a mutant, nonlethal strain of S. aureus and found that it produces a different protein, called RIP, that binds to the bacterium and prevents it from recognizing RAP. Injections of this protein in mice also reduced the occurrence of lesions.
The approach is so promising that the National Institutes of Health last month gave Panorama a $100,000 grant to begin developing a vaccine for humans. The company is also looking for drugs that might mimic the activity of RIP. But Balaban cautioned that it could be several years before clinical trials of either a vaccine or a drug might begin.
(BEGIN TEXT OF INFOBOX / INFOGRAPHIC)
A Dangerous Bacterial Foe
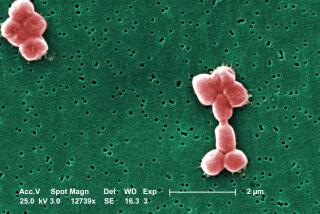
Researchers have discovered a new way to combat antibiotic-resistant Staphylococcus aureus bacteria.
Staph Infections:
The illustration at left shows how a staph-infection, in this case a skin ailment on a mouse, gains a foothold in the body of an infected animal or person.
1) Staphylococcus aureus bacteria normally produce a protein called RAP ( S . aureus bacteria proliferating on skin)
2) When there are a lot of bacteria and RAP concentrations are high, the protein binds to a receptor on the bacteria’s cell walls (cell membrane).
3) That binding activates a gene that triggers release of a dangerous toxin (gene activated to produce toxins).
****
The New Treatment:
An immunization with RAP proteins stimulates an immune response that prevents RAP from binding and heads off production of the toxin.
Source: UC Davis