Attacking Cancer’s Supply Lines
- Share via
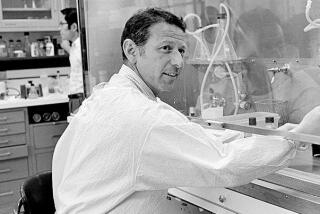
Like a proud father, Dr. Fairooz Kabbinavar stood amid a clutter of yeast tanks and half-filled vials inside the labs at UCLA’s Jonsson Comprehensive Cancer Center and shared some of his most cherished photos: pictures of mice.
Two hairless rodents--one with a neck tumor as large as its head and the other with a significantly smaller cancerous growth--strained beneath the camera lens.
“You see?” Kabbinavar said, pointing at one mouse picture then the other. “You can physically tell the difference through their skin.”
The photos, depicting mice that underwent different forms of treatment for their cancer, document Kabbinavar’s initial laboratory success with a new drug presently known as RhuMabVEGF.
The synthetic compound was developed in the South San Francisco labs of Genentech Inc. and is currently being monitored for effectiveness on Dave Musso and 98 other people around the country. The Jonsson Cancer Center at UCLA is one of eight cancer centers participating in the Genentech experiment.
RhuMabVEGF is one of about 20 experimental drugs being tested on humans that are designed to stop cancers from receiving the nutrients they need to flourish. The drug’s components neutralize a natural protein emitted by cancer cells called VEGF, short for vascular endothelial growth factor.
Scientists believe VEGF contributes heavily to angiogenesis, a biological process that allows tiny blood capillaries to form between the tumor wall and existing blood vessels in the body. The capillaries serve as lifelines to the tumors, funneling into the cancerous tissue a steady flow of body nutrients and oxygen.
Solid tumors cannot grow beyond the size of a pinhead without access to those nutrients. By eliminating the capillary lifelines, scientists developing angiogenesis inhibitors like RhuMabVEGF hope they can starve tumors and either kill them or make them more susceptible to other forms of treatment, such as chemotherapy.
Some angiogenesis inhibitors focus on VEGF, while others attack different aspects of the same capillary-forming process.
“There are many ways in which people are hoping these compounds can be useful,” said Dr. James Pluda, who oversees research on angiogenesis inhibitors for the National Cancer Institute. “They have great potential.”
But “it is important to remember the effects of these drugs are still theoretical,” Pluda cautioned.
“None of this has been proven yet.”
The idea of focusing on angiogenesis in cancer treatment was pioneered nearly 30 years ago by Dr. Judah Folkman of the Harvard Medical School and Children’s Hospital in Boston. Earlier this year, news reports of his recent success with cancer-ridden mice created a whirlwind of false hopes among cancer patients and their families that a cure for the disease would be available any day.
Scientists do not expect to be able to wipe cancer out any time soon. But they are researching hundreds of experimental compounds they hope have the potential to contain cancer.
Like the two natural protein byproducts--angiostatin and endostatin--recently discovered by Dr. Michael O’Reilly in Folkman’s laboratory, many of those agents have successfully reduced or eliminated tumors in mice. But--unlike RhuMabVEGF--they have yet to be deemed fit for human clinical trials.
As Kabbinavar put it: “It is a big leap . . . between mouse and man.”
Kabbinavar--both a clinical doctor and an oncologist at the UCLA Jonsson Comprehensive Cancer Center--is among the few so far who have made that leap.
In 1992, he and Dr. Dennis Slamon, head of all clinical research at UCLA, saw their first success in laboratory mice with what eventually became RhuMabVEGF. The drug was derived from a mouse antibody discovered by Genentech scientist Napoleone Ferrara that appears to stop VEGF from forming capillaries between tumors and existing blood vessels.
Kabbinavar and Slamon injected the antibody into mice with lung cancer. They then combined their treatment with traditional chemotherapy, something oncologists during the early 1990s had not yet tried with angiogenesis inhibitors.
The results were exponentially greater than that of chemotherapy or the antibody injected alone, Kabbinavar said.
As shown in his lab photos, mice treated solely with chemotherapy had tumors that were as large or larger than when the experiment started, Kabbinavar said. Meanwhile, identical tumors on mice treated with a combination of chemotherapy and the anti-VEGF agent shrank rapidly.
“Right from the first experiment, when we saw the results, we were excited,” he said. “We remain cautiously optimistic. In a lab setting, you have to be careful about getting too excited.” When additional tests for ovarian, colon, breast and head and neck cancers confirmed the mouse antibody’s effectiveness, Genentech scientists altered its DNA structure in 1997 to make it compatible with the human system for clinical trials.
Until the trials are complete for Musso and hundreds of others expected to participate in anti-angiogenic experiments during the next several years, the true impact of these agents will not be known.
Scientists are still uncertain whether the drugs could seriously hamper a patient’s ability to heal bleeding wounds or--in pregnant women--the ability of a fetus to fully develop. Those and a few other biological functions also rely on angiogenesis.
Should those potential side effects not develop, or prove tolerable, the excitement about RhuMabVEGF and other angiogenesis inhibitors may be hard to contain, even though it could take up to seven years for any of the substances to hit the market.
“Up until now, we have learned every which way we can fail” in treating most forms of cancer, Kabbinavar said.
“It is our firm belief that all solid tumors and even [blood] malignancies [like leukemia] need blood supplies to flourish,” he said. “Anti-angiogenic therapy . . . will become a part of the cancer regimen for all different types of malignancies.
“Is there a cure in sight? Probably not,” Kabbinavar said. But, “We may soon be able to accomplish better control of the disease with less side effects. That is almost as good.”
(BEGIN TEXT OF INFOBOX / INFOGRAPHIC)
New Hope in Battling Cancer
A synthetic compound called RhuMabVEGF is being tested on 99 patients at medical centers around the country, including the Jonsson Comprehensive Cancer Center at UCLA. The compound was designed to interrupt the natural cycle of protein, VEGF, that plays an important role in allowing cancerous tumors to grow.
*
VEGF’s destructive cycle:
A cancerous tumor emits VEGF cells that attach themselves to blood vessels. The cells cause vessels to grow branches toward the tumor.
*
When the branches reach the tumor, they supply it with nutrients and oxygen. The tumor then begins to grow rapidly.
*
Anti-VEGF treatment:
RhuMabVEGF binds to VEGF
RhuMabVEGF binds to the natural VEGF, preventing the cells from attaching to blood vessels.
*
The tumor is unable to increase its pathways to nutrients, and can thus be attached successfully by chemotherapy treatments.
Sources: UCLA’s Jonsson Comprehensive Cancer Center and Genantach Inc.