Schizophrenia Drugs Comparable, Study Shows
- Share via
A study comparing schizophrenia drugs has found that an older medication, perphenazine, is as effective at managing the devastating brain disorder as most of the newer, more expensive drugs.
The study also found that one newer drug, olanzapine, was modestly more effective than the four other medications in the trial but also carried the greatest risk for the serious side effects of obesity and abnormal blood levels of sugar and fat.
The findings, announced Monday, provide psychiatrists with their first direct comparison of the antipsychotic medications, gathered over a reasonably long period of time, in real-life patient settings.
But the trial also made it plain that medications for schizophrenia are far from ideal.
By the end of the 18-month study, 74% of the patients had stopped taking the drug they had been assigned. Even in the most successful case of olanzapine, 64% of the patients had dropped the drug for another one before the 18 months were up, the researchers reported in their study, to be published this week in the New England Journal of Medicine.
“Seventy-four percent is a breathtaking number,” said Dr. Ken Duckworth, medical director for the National Alliance on Mental Illness, an Arlington, Va.-based patient advocacy group. “We need to create better treatments and think more creatively about ways to support people in taking medicines that may help them.”
Schizophrenia affects an estimated 3.2 million Americans, causing them to experience hallucinations and paranoid delusions.
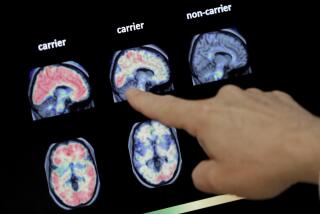
Since the 1950s, a class of drugs known as antipsychotics have been used to treat these symptoms. The drugs act by blocking the action of a key brain protein known as the dopamine D2 receptor.
However, this first wave of drugs, including perphenazine, also cause troublesome side effects such as tremors, rigidity, muscle restlessness and involuntary limb movements.
In the 1990s, a new group of so-called atypical antipsychotic drugs entered the market. The drugs were believed to have lower rates of body-movement side effects.
Today, more than 90% of the antipsychotics prescribed to people with schizophrenia are atypicals, which are far more expensive.
Olanzapine, for example, costs about $600 a month at higher doses, compared with $50 a month for perphenazine.
Sales of antipsychotics in the United States total about $10 billion a year. Starting in 1999, the federally funded trial enrolled more than 1,400 adults at 57 sites around the country.
Patients were randomly assigned to receive either the older drug perphenazine or one of four atypicals: olanzapine (brand name Zyprexa), quetiapine (Seroquel); risperidone (Risperdal) or ziprasidone (Geodon).
At the dosages chosen, perphenazine was equally as effective as quetiapine, risperidone and ziprasidone, as defined by how long patients stayed on the drugs, the study found.
Staying on drugs is a general measurement that factors in the satisfaction of both patient and doctor about a drug’s effectiveness and its side effects. It is especially significant for people with schizophrenia, who often think they don’t need treatment.
Surprisingly, movement disorders were no more apparent with perphenazine than with the atypical drugs.
The findings may help doctors decide which drug to choose first for a patient, said Dr. Jeffrey A. Lieberman, chairman of the department of psychiatry at Columbia University Medical Center and principal investigator for the study.
For instance, a patient whose symptoms are hard to control might be a good candidate for olanzapine, he said. Another patient whose symptoms are more manageable might be better suited to a drug with lower risk of obesity and abnormal blood levels of sugar and fat.
Even though the new drugs are more costly, other expenses such as hospitalizations during relapses must be factored into the cost-benefit equation, the authors said.
Patients receiving olanzapine experienced fewer such hospitalizations during the trial.
The researchers said that data from the trial will also be used to examine cost-effectiveness of the drugs and their effect on cognitive abilities and quality-of-life issues, such as the ability to work and live independently.