The other drug war
- Share via
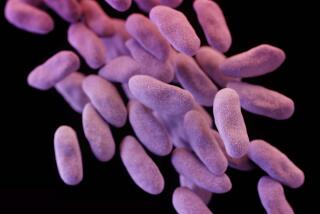
METHICILLIN-resistant Staphylococcus aureus -- that infamous, life-threatening microscopic germ also known as MRSA -- is not the only microbe we should fear. On March 1, the Infectious Disease Society of America warned of at least six dangerous bacterial and fungal strains, responsible for diseases such as pneumonia and wound and bloodstream infections, that have been acquiring resistance to antibiotics, including last-line drugs such as vancomycin and imipenem.
They say the U.S. is facing a serious healthcare crisis if replacement drugs aren’t found. They note that few large drug firms are looking for them, for there is not much profit in the search. Nevertheless, some drug companies and academics are continuing to seek, and sometimes find, new antibiotics that can fight bacteria -- gleaned from the soil, the ocean and the forest floor, from lichens, seaweed and laboratory tinkering. Today, IDSA estimates that about a dozen antibiotics are in late clinical testing.
The first antibiotic, discovered by British microbiologist Alexander Fleming in the 1920s, was derived from a mold (Penicillium notatum) that he found growing in a dish in his lab. Since Fleming’s time, the traditional source of antibiotics has been soil-dwelling bacteria and fungi.
But these days, searching the old way leads to rediscovering the same antibiotics over and over again, says Dr. Francis P. Tally, chief scientific officer of the Lexington, Mass.-based company, Cubist Pharmaceuticals. “You’d keep describing the same wheel again,” Tally says.
Companies and university labs are having to stretch their imaginations.
Cubist Pharmaceuticals hasn’t given up on the soil. It’s seeking microbes that are so rare that they have been overlooked. To find them, the company has constructed bacteria that are resistant to most known soil antibiotics, so that only novel compounds can kill them in tests. Tally says the approach has yielded promising bacteria -- and 70% of these have never been described before.
But 99% of soil dwelling bacteria can’t be grown in a lab, says Julian Davies, a microbiologist at the University of British Columbia in Vancouver. Many antibiotics might exist there, unknown by science, because the bugs that produce them are too finicky to be cultured.
Davies and others have tried to circumvent the culturing problem not by growing the bugs, but by isolating their genes instead. They then test the ability of these genes to produce antibiotics. But so far, Davies says, success has been limited, in part because it’s difficult to harvest large enough pieces of DNA from soil.
Davies is studying bacteria that grow on lichens -- and there he’s had more luck. He’s isolated about 2,000 bacterial strains that grow on lichens, and probably half have antibiotic activity, he says.
Seaweeds are the source of choice for Brian Austin, a microbiologist of Scotland’s Heriot-Watt University in Edinburgh. He’s coaxed bacteria that grow on them to produce antibiotics, but only after using a trick: He cultured them on a household sponge from his local supermarket.
Oceanographer William Fenical of the Scripps Institution of Oceanography in La Jolla, Calif., also favors the sea. But in his case, he’s looking for antibiotic-producing bacteria in the mud at the bottom of the ocean, a place still barely explored by science. Already, he says, he has identified dozens of strains with antibiotic activity.
Some companies, such as Johnson & Johnson, have been trying to develop antibiotics by chemically modifying known ones in the lab. But that approach has its limits, some say, in part because there are only so many ways to modify these compounds, and the result is antibiotics that act similarly to the ones they started with.
And so Pfizer Inc. and other firms are trying a different approach: They’re using the recent accumulation of genetic information of many disease-causing bacteria to find new compounds, and new parts of bacteria, to attack. The scientists destroy bacterial genes, one by one, to find ones that the bugs need to survive. Then they test millions of synthetic chemicals to find ones that interfere with the products of those genes. Using this approach, Pfizer has a number of promising chemicals, and next year plans to start early clinical trials in humans with three or four compounds.
Meanwhile, the Danish company Novozymes is focusing on short proteins called antimicrobial peptides that humans and other animals produce on their skin, and gut and lung surfaces, to fight infection. It isolated one such peptide, Plectasin, from a fungus found on the floor of European pine forests. And the Philadelphia-based company PolyMedix has made artificial molecules with similar properties to some natural, antimicrobial peptides.
Both companies say that injecting these drugs into animals can fight MRSA infections, and PolyMedix plans early clinical trials as soon as next year.
But some scientists fear that if bacteria become resistance to these drugs, they may resist people’s natural defenses.
Despite these new leads, infectious disease experts say there’s no call for complacency. Dr. Brad Spellberg, an infectious disease specialist at Harbor-UCLA Medical Center in Torrance, has reported about a 60% decline in the number of FDA-approved antibiotics since the mid-1980s. And it can easily take a decade of animal and human trials before a new compound is ready to be sold as a drug.
Meanwhile, 90,000 people die from hospital infections every year, 70% of them from drug-resistant bacteria including MRSA, according to the Centers for Disease Control and Prevention.
“That’s about the equivalent of two Vietnam Wars,” Spellberg says. “It makes bird flu look like a joke.”
*
(BEGIN TEXT OF INFOBOX)
The bug’s life
The development of resistance in bacteria is evolution in action. Bacteria take just 20 minutes to divide, which means lots of generations are spawned in a short time.
Every division of the bug’s DNA can come with mistakes -- and these mistakes sometimes lead to changes that enable a bacterium to survive an antibiotic.
If the antibiotic is used a lot, those rare resistant bugs will be able to grow when other ones won’t, and will come to represent more and more of the bacterial population.
Antibiotics act in various ways: They often inhibit proteins that bacteria need to synthesize something, such as the cell wall, DNA or proteins.
They commonly interfere with the action of these key proteins by binding to them.
Some bacteria develop resistance by changing their proteins so that the antibiotics can’t bind to them anymore. Others develop enzymes that destroy the antibiotic, or simply transport the antibiotic out of the cell.
The easiest way bacteria develop resistance is by having sex: That’s when bacteria exchange genetic material, including genes for antibiotic-resistance.