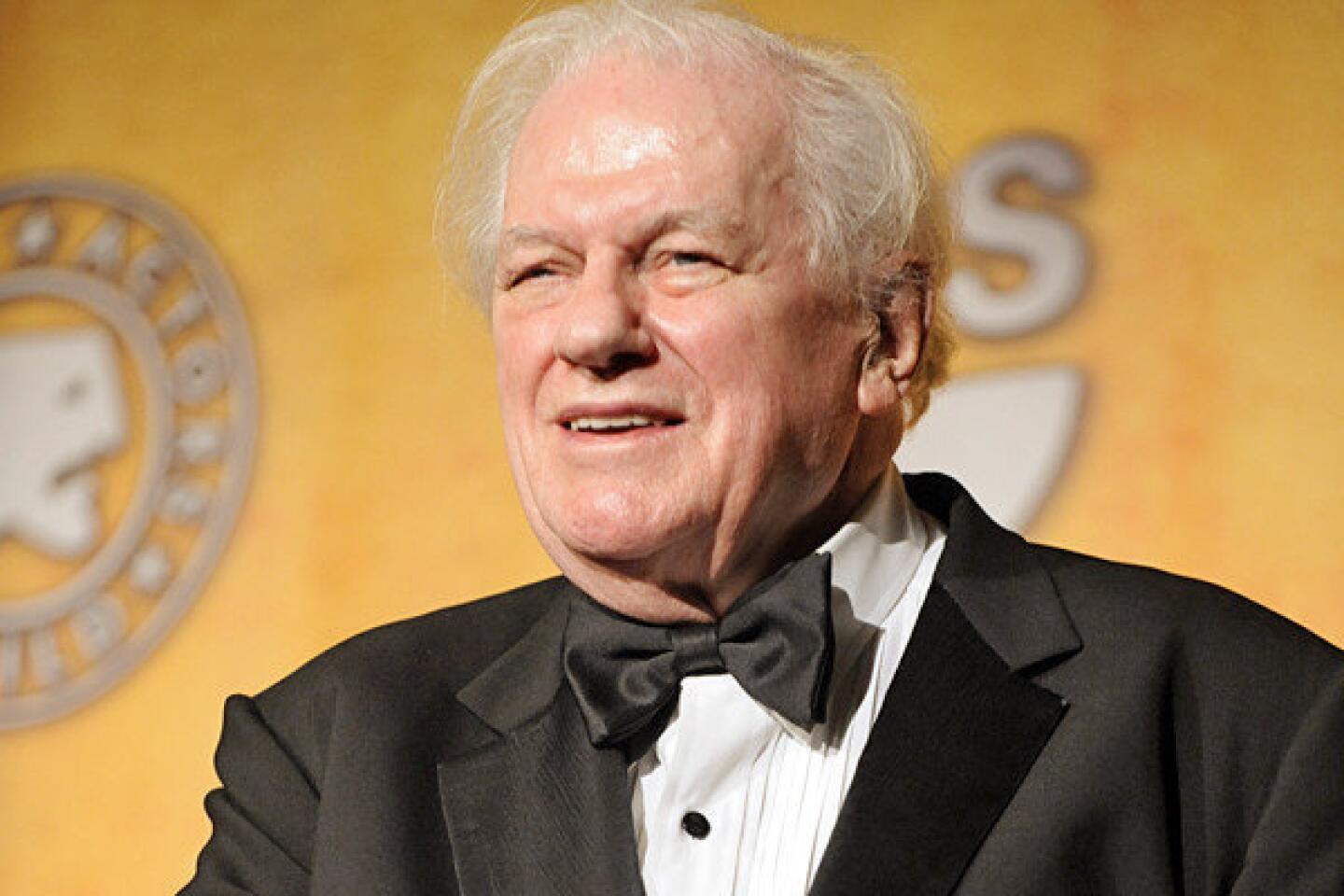
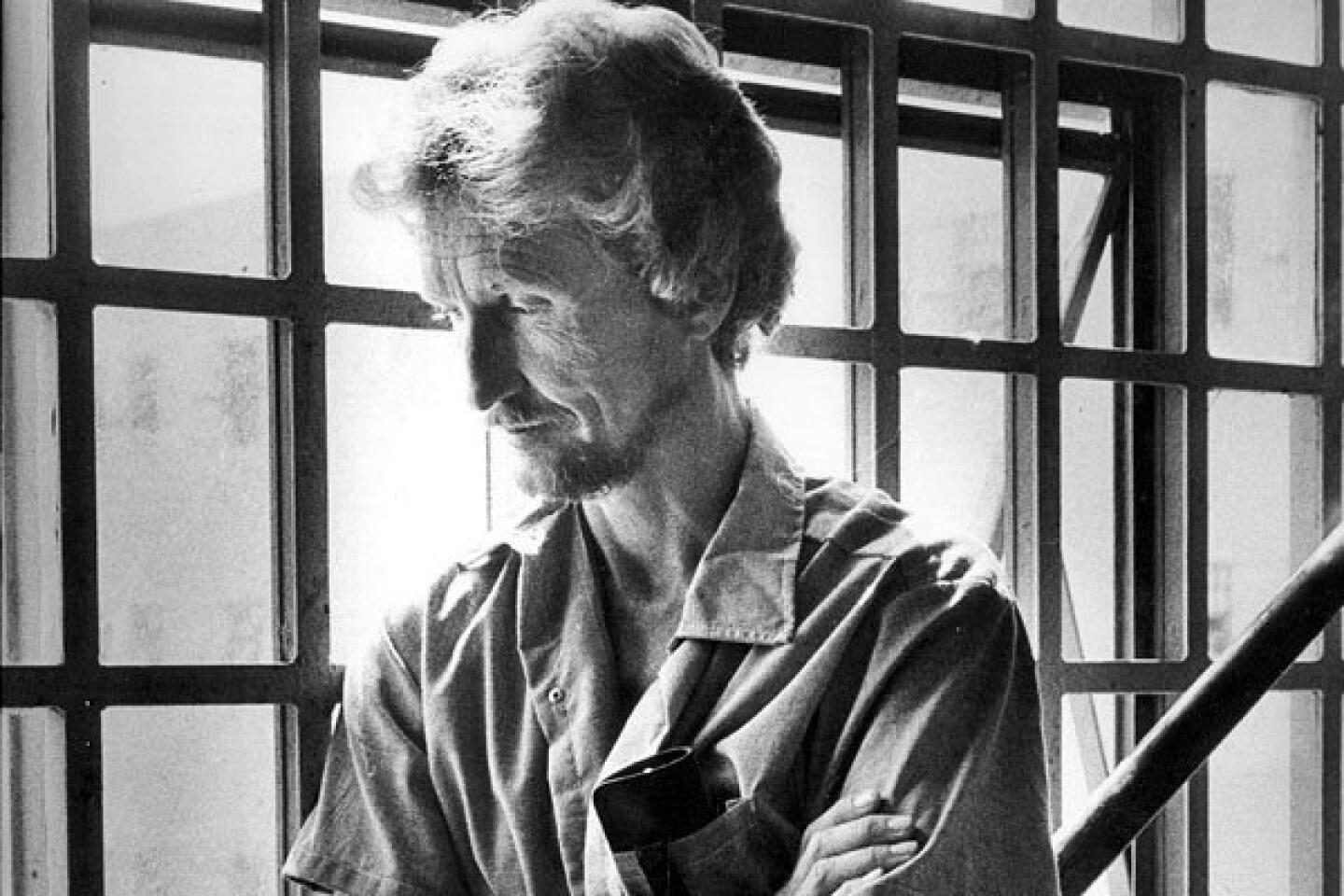
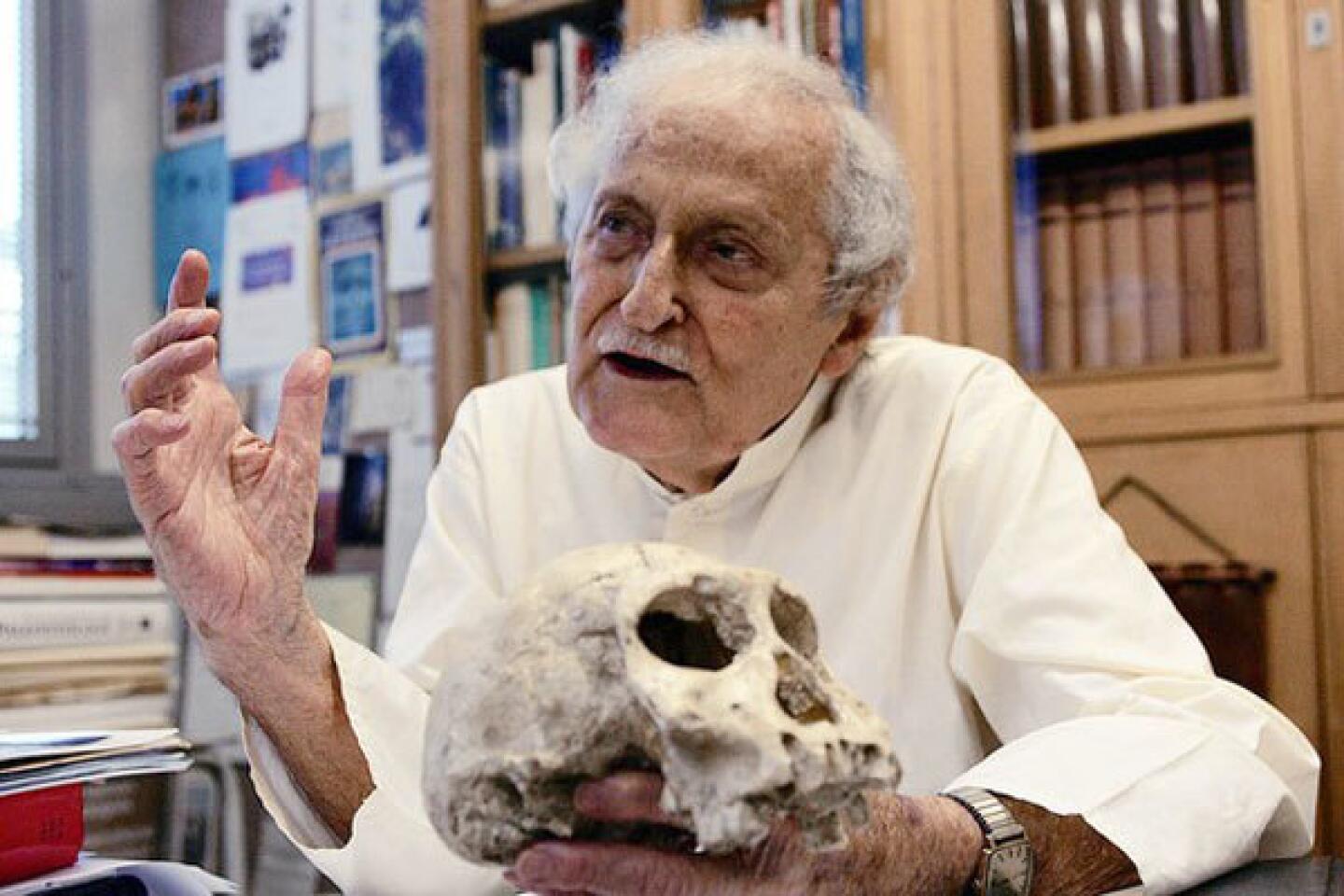
Dr. Paul H. Crandall dies at 89; invented techniques for diagnosing, treating epilepsy
- Share via
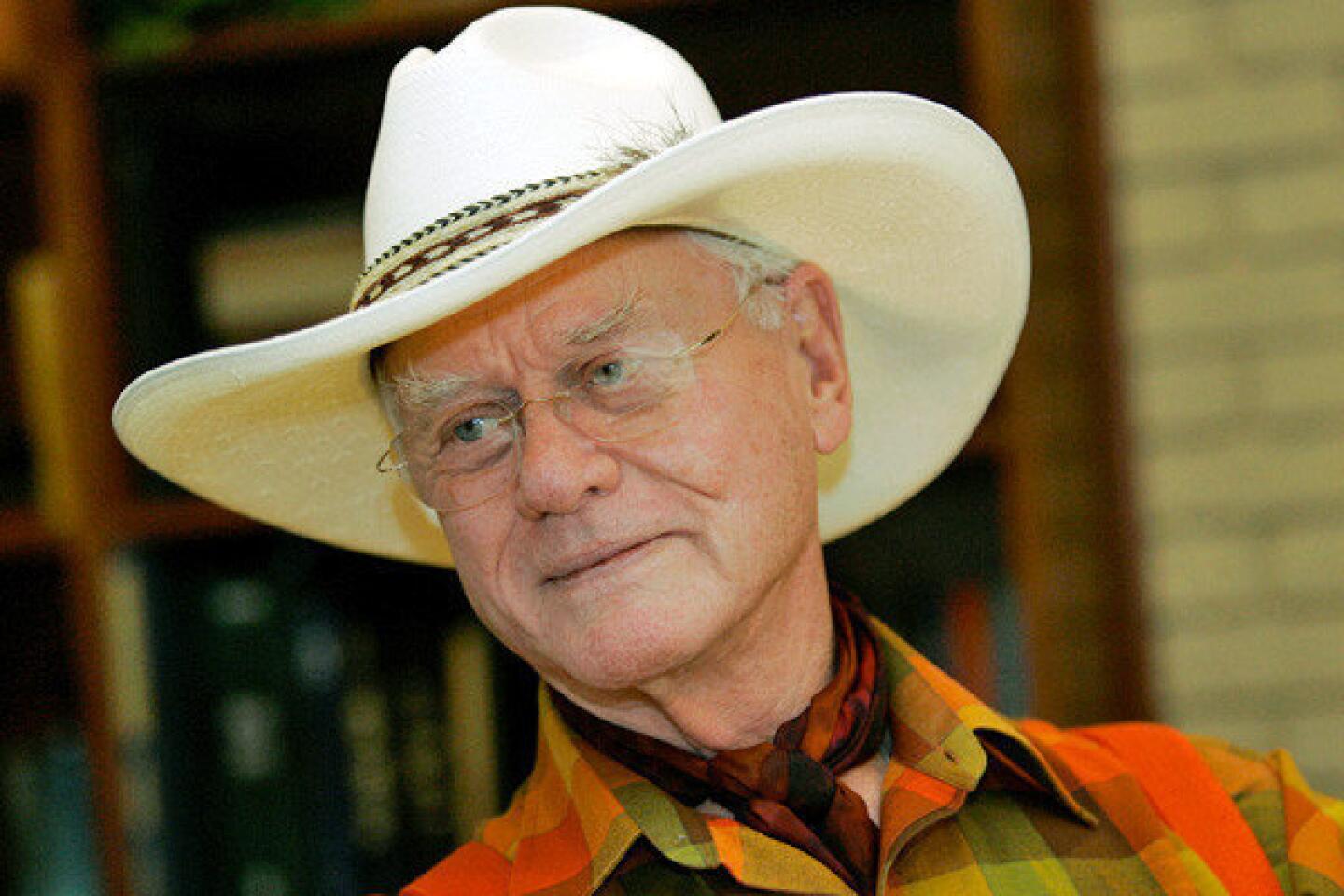
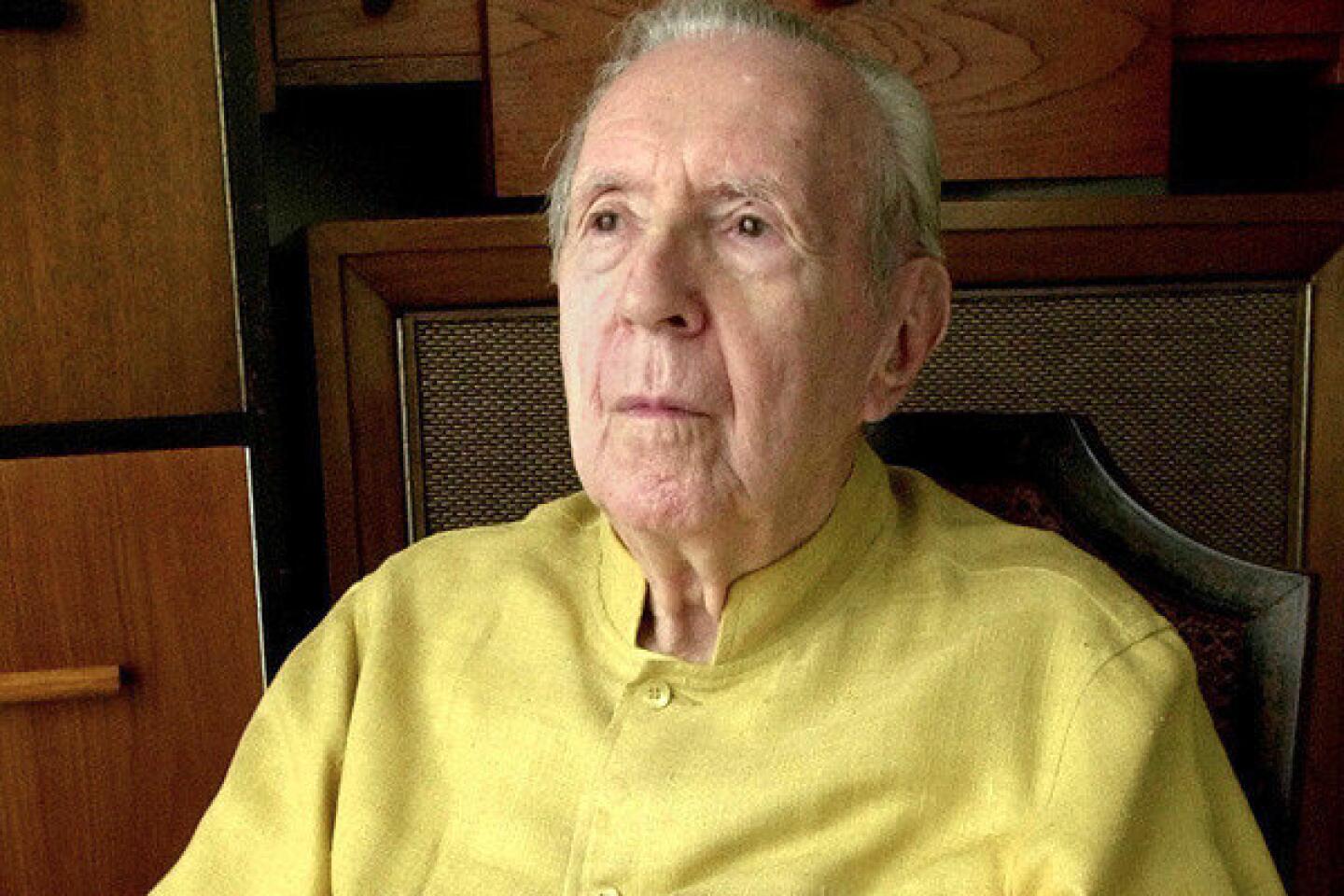
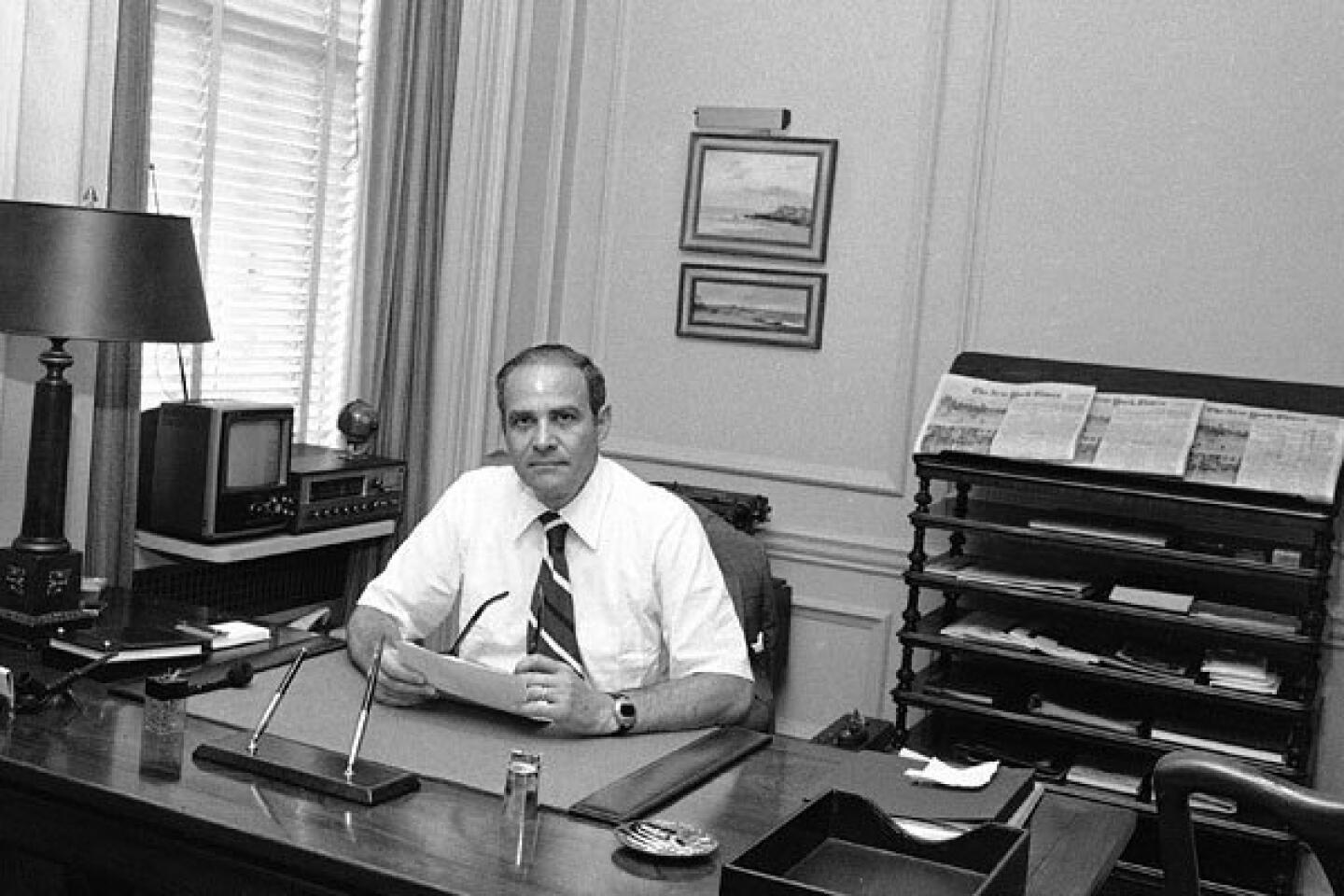
Dr. Paul H. Crandall, a UCLA neurosurgeon who pioneered now widely used techniques for diagnosing the source of epileptic seizures in the brain and removing the offending cells, died March 15 from complications of pneumonia at Santa Monica-UCLA Medical Center. He was 89.
Crandall, who founded the UCLA Department of Neurosurgery, “was the father of UCLA’s epilepsy program,” Dr. Neil Martin, the current chairman of neurosurgery at UCLA’s Geffen School of Medicine, said in a statement. “His clinical work laid the foundation for our current strategies to treat epileptic seizures, and his scientific research informs neurosurgeons’ treatment of epilepsy today.”
Epilepsy can be treated with drugs in about 60% of cases. Surgeons have been attempting to cure other seizures with brain surgery since at least the late 19th century, but doctors often removed massive amounts of tissue without having any understanding of where in the brain the seizures were actually originating.
Researchers in France had attempted to implant electrodes in the brain to record brain activity during seizures, but the electrodes were left in only during the operation itself and provided only minimal information.
Crandall and Dr. Richard Walter, then head of neurology at UCLA, perfected the ability to implant electrodes in the brains of epileptic patients and leave them for extended periods. Beginning in the early 1960s, patients were brought into the laboratory each day and hooked up to an EEG machine that recorded electrical impulses on paper strips, producing mounds of paper. But the researchers failed to capture any seizures.
Crandall happened to be watching one of NASA’s early Gemini orbital missions on television when he heard mission control announce the astronaut’s heart rate. Intrigued, he called NASA and asked how they did it. He was told that the agency used a newly opened FM radio band, putting several channels of information on an FM frequency that was then beamed back to Earth. He immediately asked for one of the devices.
After nearly two years of negotiations, NASA sent him an FM telemetry device, which allowed him to hook up a patient’s brain electrodes to a small transmitter. The signal was then recorded on a reel-to-reel tape recorder, allowing 24-hour monitoring. Crandall captured his first seizure in 1968. Later, the team added video recording to correlate patient behavior with brain activity.
By embedding the electrodes at the same sites in every patient, Crandall’s team was able to gradually focus on groups of cells where abnormal activity was occurring, allowing removal of the cells and mitigating seizures. And by removing clumps of cells intact, researchers were able to study in the laboratory how interactions of the cells produced seizures.
His team developed the protocol and the nomenclature that is still used by neurosurgeons to treat epilepsy: Phase 1, a normal EEG with surface electrodes to diagnose epilepsy; Phase 2, use of implanted electrodes to localize affected cells; and Phase 3, surgical removal of the cells.
“His contribution is not just what he found, but also the approach of how to go about doing this,” said Dr. Gary Mathern, a UCLA professor of neurosurgery.
Paul Herbert Crandall was born Feb. 15, 1923, in Essex Junction, Vt., the youngest of seven children. He received his bachelor’s degree from the University of Vermont in 1943, then joined the U.S. Army, where he was chosen to attend medical school, receiving his medical degree from Vermont in 1946. After a residency at the University of Chicago, he rejoined the Army Medical Corps in 1952, serving two years as chief of neurosurgery at a military hospital in Frankfurt, Germany.
In 1954, he arrived at UCLA, where he was one of three founding members of the neurosurgery division, which was upgraded to a department in 2008. He retired in 1988 but continued his research.
Crandall served on the U.S. Department of Health’s National Commission for Epilepsy from 1976 to 1977. Because his work had demonstrated the value of long-term monitoring of seizures and of his procedures for managing difficult cases, the commission recommended the establishment of specialized epilepsy centers in major urban areas, a recommendation that was subsequently implemented.
His work also helped extend surgery to children for controlling seizures.
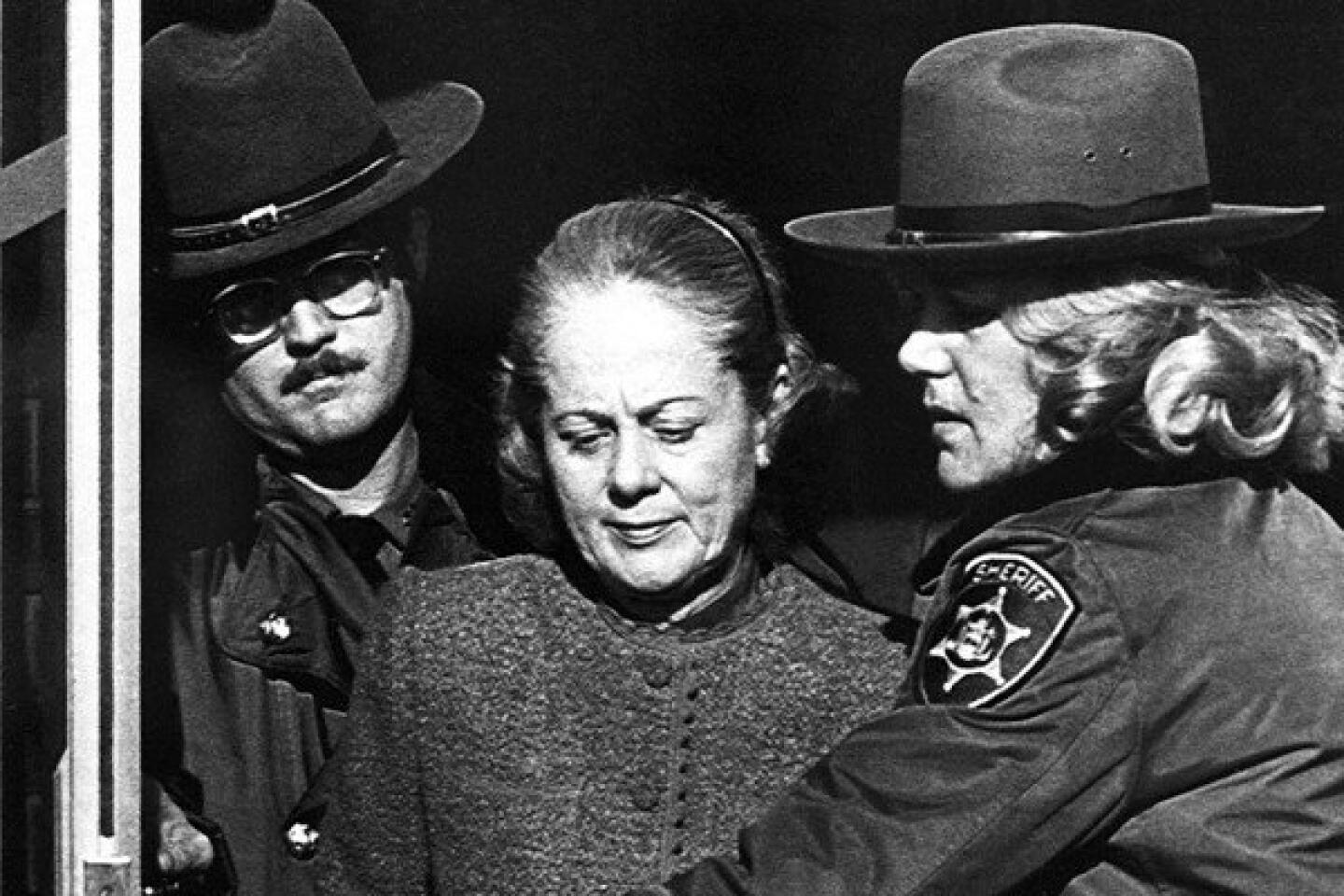
In 1977, Crandall performed surgery on 18-year-old Alfonsina “Nina” Davies whose parents had searched futilely for a cure for her severe epilepsy. The surgery halted the seizures and Nina completed college, earning a doctoral degree in education and becoming an assistant superintendent for the Santa Ana Unified School District. Unfortunately, she died in 2011 of a condition known as sudden unexplained death in epilepsy, a rare outcome of the disease.
In October 2011, her parents, Thomas and Nadia Davies, donated $2 million to UCLA for epilepsy research, endowing a chair in Crandall’s honor.
Crandall is survived by his wife, Barbara, a UCLA professor emeritus of pediatrics and genetics; four children; and three grandchildren.
Maugh is a former Los Angeles Times medical writer.
More to Read
Start your day right
Sign up for Essential California for the L.A. Times biggest news, features and recommendations in your inbox six days a week.
You may occasionally receive promotional content from the Los Angeles Times.