‘Zero pain is not the goal’ of medical treatment, doctors say
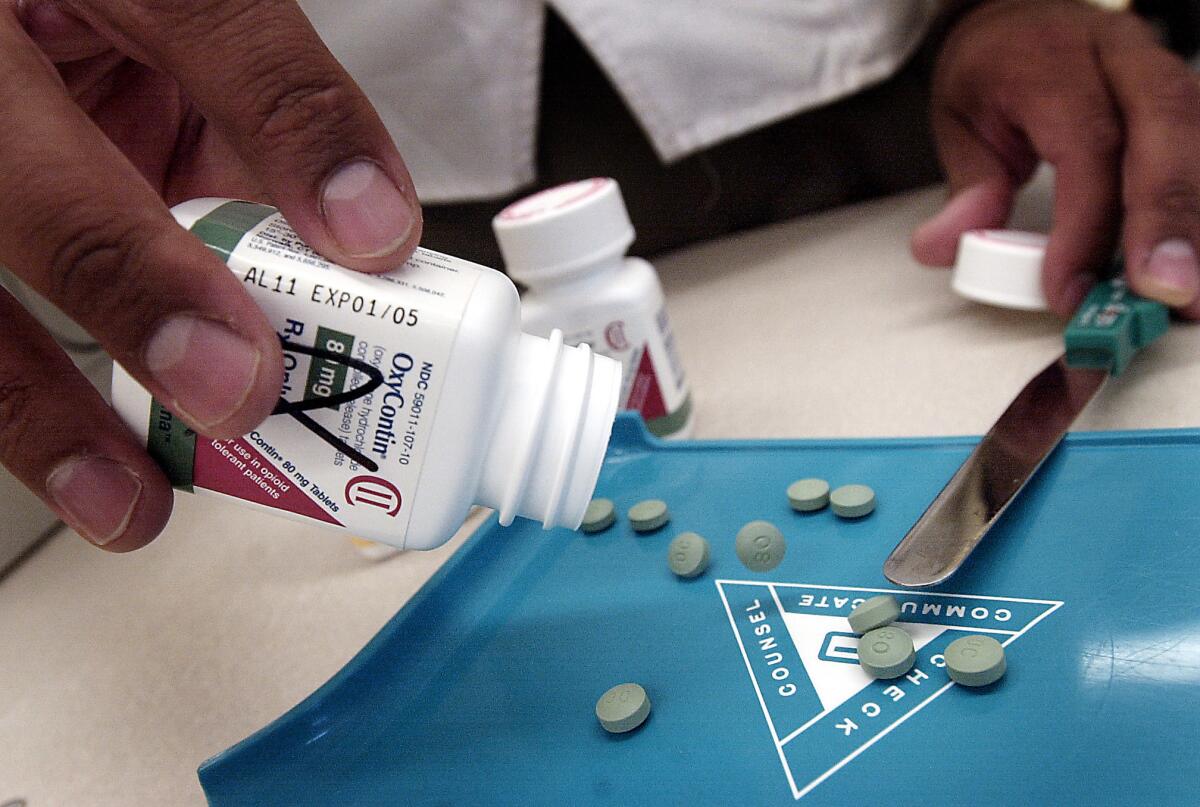
A pharmacist counts OxyContin pills. With the Centers for Disease Control and Prevention urging doctors to refrain from prescribing opiate painkillers to patients with chronic pain, some physicians are making the case that reducing pain to zero should not be the goal of treatment.
- Share via
As doctors contemplate a future without opiates to treat chronic pain, some are making the case that eliminating their patients’ pain is not only impossible, it’s unnecessary.
“Zero pain is not the goal,” Dr. Thomas H. Lee, chief medical officer of the healthcare consulting firm Press Ganey, wrote in a commentary published Tuesday in the Journal of the American Medical Assn. “The reduction of suffering is — and that is something more complex than analgesia alone.”
That view flies in the face of attempts by doctors to suppress their patients’ pain as much as practically possible. These efforts helped fuel a surge in prescriptions for opiate painkillers, such as OxyContin, Percocet and Vicodin.
See more of our top stories on Facebook >>
The popularity of these medications has been blamed for surging rates of opiate addiction and death in the United States, prompting the Centers for Disease Control and Prevention to issue new guidance urging doctors to reserve the medications for patients with acute cancer pain, those receiving palliative care and those in their final days of life. For treatment of chronic pain due to conditions like arthritis and back problems, doctors instead should try Tylenol, Advil or other non-addictive therapies, the guidelines recommend.
For most patients, the benefits of opiate painkillers are “unproven and transient,” said Dr. Tom Frieden, director of the CDC. However, the drugs can be “just as addictive as heroin,” he said.
More than 165,000 people in the U.S. have suffered fatal overdoses of these prescription painkillers since 1999, according to the CDC. About 1.9 million patients are estimated to be addicted to or abusing the drugs.
Those harms must be weighed against some rather dubious benefits, Frieden and Dr. Deborah Houry, director of the CDC’s National Center for Injury Prevention and Control wrote in a commentary published Tuesday in the New England Journal of Medicine.
They noted that several studies, conducted on post-surgical patients and on menopausal women with chronic pain conditions, suggest that long-term opioid use often fails to bring relief. In fact, these drugs may actually worsen patients’ pain and lower their functioning, possibly by magnifying the subjective experience of pain.
While healthcare’s clear purpose has always been the reduction of suffering, patients understand the distinction between that goal and the elimination of pain, Lee wrote in JAMA.
Suffering includes more than physical pain; it also encompasses functional impairment, fear, uncertainty and confusion, he wrote. When doctors listen to and communicate with patients, show compassion and skill, and coordinate with other physicians to address patients’ needs, suffering is reduced – even if they still have pain.
“Quality does not mean the elimination of death,” Lee wrote. “And compassion for patients does not mean the elimination of all pain.”
In a guide to fellow physicians, Dr. Mitchell Katz, director of the Los Angeles County Department of Health Services, wrote that when he sees chronic pain patients, he may ask them to rate their pain on a scale of 1 to 10, but he places much more weight on how well they are able to function.
“When a patient tells me that the opioid enables them to sleep at night, get out of bed and do their usual activities, I feel much more reassured than I do by the patient report of any pain score,” he wrote in JAMA Internal Medicine.
Follow us on Twitter @LATMelissaHealy and @LATkarenkaplan and “like” Los Angeles Times Science & Health on Facebook.
MORE SCIENCE & HEALTH NEWS
These newly discovered bacteria can eat plastic bottles
NFL executive acknowledges a link between football-related head trauma and CTE
Vaccination aversion has fueled measles and whooping cough outbreaks, study finds





