Column: New-age medicine star Andrew Weil defends UC Irvine against charge that it’s partnering with quacks
- Share via
Dr. Andrew Weil, perhaps the nation’s best-known purveyor of “New Age” medicine, has written The Times to “take umbrage” at my recent column warning that UC Irvine risks becoming a haven for quacks if it’s not careful about deploying a $200-million gift from the Samueli family.
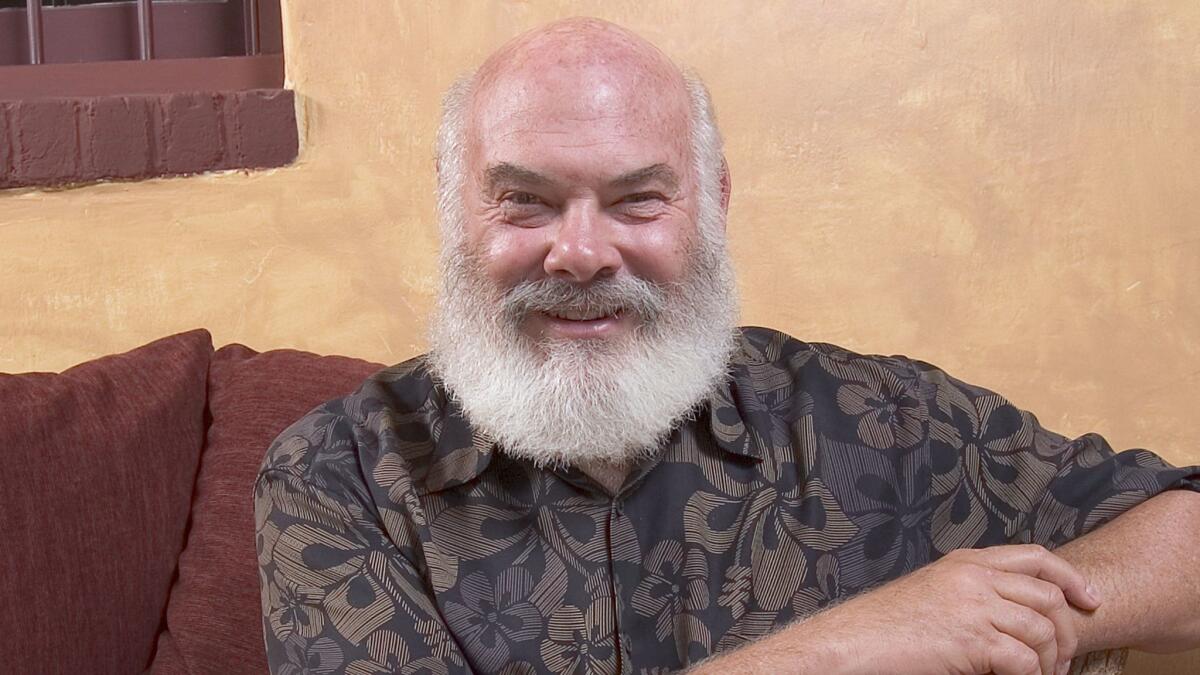
Weil, whose familiar bearded visage peeks out from covers of his more than 20 published books, desires to make a distinction between “quackery,” which “refers to dishonest practices performed by those who pretend to have special knowledge and skill in some field,” and what he does at his Center for Integrative Medicine at the University of Arizona.
Real integrative medicine, he says, is “healing-oriented medicine that reaffirms the importance of the relationship between practitioner and patient, focuses on the entire patient and body systems, is informed by evidence, and makes use of all therapeutic and lifestyle approaches to achieve optimal health and healing.”
If IM were so science-based and transforming health care so much without quackery, you’d think [Weil] could have come up with more compelling examples.
— David Gorski
Fair enough. But then why does Weil exaggerate, in the very same letter to the editor, the level of professional acceptance of some of his “integrative” nostrums? (Weil’s letter is co-signed by three of his acolytes at his center and a recent graduate, as if to suggest there’s strength in numbers even if everyone’s a member of the same family.) Weil says integrative medicine, presumably as he practices it, is “informed by evidence.” But the evidence he cites in his letter isn’t very convincing.
Before we delve further, some background: Henry and Susan Samueli, whose multibillion-dollar fortune springs from his co-founding of the semiconductor firm Broadcom, are sworn adherents of integrative medicine, including homeopathy, which has been scientifically discredited.
Some of their huge gift will go to fund a building for the Samueli College of Health Sciences, which will incorporate UC Irvine’s medical and nursing schools and planned schools of pharmacy and “population health” (that is, public health). But most of the money will be devoted to an endowment for up to 15 chairs for world-class faculty with “expertise in integrative health” and for the training of students in that curriculum.
As I reported last month, medical professionals who believe that healthcare should be based on treatments validated by science view the very term “integrative medicine” as a path to introduce unproven or disproven therapies into medicine. UC Irvine has hewed very close to that line in relation to an earlier gift from the Samuelis, which was used to fund a center at the university that actually offered homeopathy to patients. (The mention of homeopathy disappeared from one of the college’s web page after I asked about it; but a naturopath on the staff is still promoting homeopathy under the UC Irvine imprimatur even now.)
Promoters of integrative medicine often play a couple of shell games with the public. First, they assert that conventional doctors treat only discrete diseases in isolation, while integrative medicos approach health “holistically.” This is what Weil is up to when he writes in his letter that his method “reaffirms the importance of the relationship between practitioner and patient [and] focuses on the entire patient and body systems.” The distinction is absurd, of course, as it’s hardly uncommon for any patent to be queried by his or her doctor about lifestyle, diet, home environment and so on.
“IM proponents didn’t invent the doctor-patient relationship, or looking at patients as whole people, or lifestyle factors’ influence on health,” observes Steven Novella of Yale Medical School, a prominent critic of integrative medicine.
The other trick is to describe integrative medicine entirely in terms of recommendations that traditional doctors find unobjectionable or salutatory, such as good diet and exercise, but downplay dubious therapies such as “energy healing,” naturopathy and homeopathy. “The problem, of course, is what the definition leaves out,” says David Gorski of Wayne State University’s medical school, a fellow skeptic with Novella, “namely how much quackery finds its way into integrative medicine along with the exercise, nutrition, and the like.”
Then there’s the overstatement — or even misrepresentation — of the current level of scientific acceptance of “integrative” treatments. That brings us to Weil’s references to the American Heart Assn., which he quotes as stating that meditation “may be considered a reasonable adjunct to guideline-directed cardiovascular risk reduction,” and the American College of Physicians, which he asserts “recommends acupuncture and mind-body approaches for low back pain.”
The truth is that neither of these citations amounts to the full-throated endorsement of these treatments implied in Weil’s letter. The American Heart Assn. statement, issued Sept. 28, generally treats meditation as innocuous — it says meditation doesn’t seem to do any harm and doesn’t cost much money, so there’s no particular reason for “those interested in this lifestyle modification” not to try it. But of studies purporting to establish the benefits of meditation, the association cautions that “the overall quality and, in some cases, quantity of study data are modest. It advises that patients be made to understand that the benefits of meditation “remain to be better established.”
As for the American College of Physicians’ recommendation on acupuncture, it’s similarly equivocal. The ACP issued its guidelines for treatment of low back pain in April. The doctors said that in most cases, the best therapy for the pain is time, “regardless of treatment.” If you must treat, the guidelines say, heat is the preferred non-drug approach, but it’s supported by only “moderate-quality evidence.” Treatment with acupuncture, along with such other approaches as massage or spinal manipulation is supported only by “low-quality evidence.” There’s better evidence for acupuncture for chronic low-back pain, but even there the evidence is “moderate quality.”
Once again, hardly a ringing endorsement.
That raises the question of what else Weil has to support his claims for integrative medicine. The paucity of evidence isn’t lost on critics such as Gorski, who says it’s “rather telling that the best examples Dr. Weil could come up with were an ACP recommendation for acupuncture based on weak evidence and a very lukewarm ‘may’ recommendation from the AHA for meditation to reduce risk of heart disease.
“If IM were so science-based and transforming healthcare so much without quackery,” Gorski adds, “you’d think he could have come up with more compelling examples.”
That’s the problem with so much of what falls under the umbrella of integrative medicine. What’s useful in the category doesn’t need to be labeled “integrative” — it’s part of accepted medical practice. What’s novel and unusual consistently turns out to be unproven or even disproven. IM advocates often depict the lack of proof for the efficacy of their methods as a virtue — as if there are benefits, but they just haven’t been found yet, and no news is good news.
That won’t do in a medical setting, and shouldn’t be acceptable at UC Irvine. Why should Andrew Weil and his associates take “umbrage” at my pointing that out?
Keep up to date with Michael Hiltzik. Follow @hiltzikm on Twitter, see his Facebook page, or email michael.hiltzik@latimes.com.
Return to Michael Hiltzik’s blog.







