Black patients fare better than whites when both get same healthcare, study finds
A nine-year study of more than 3 million veterans found that when black patients and white patients received the same level of healthcare, blacks fared better than whites.
- Share via
On most health measures, blacks fare much worse than whites — differences that have largely been attributed to socioeconomic factors, access to healthcare and discrimination by doctors in the treatments they prescribe.
But if there were a health system in which all patients basically got the same care, would the disparities still exist?
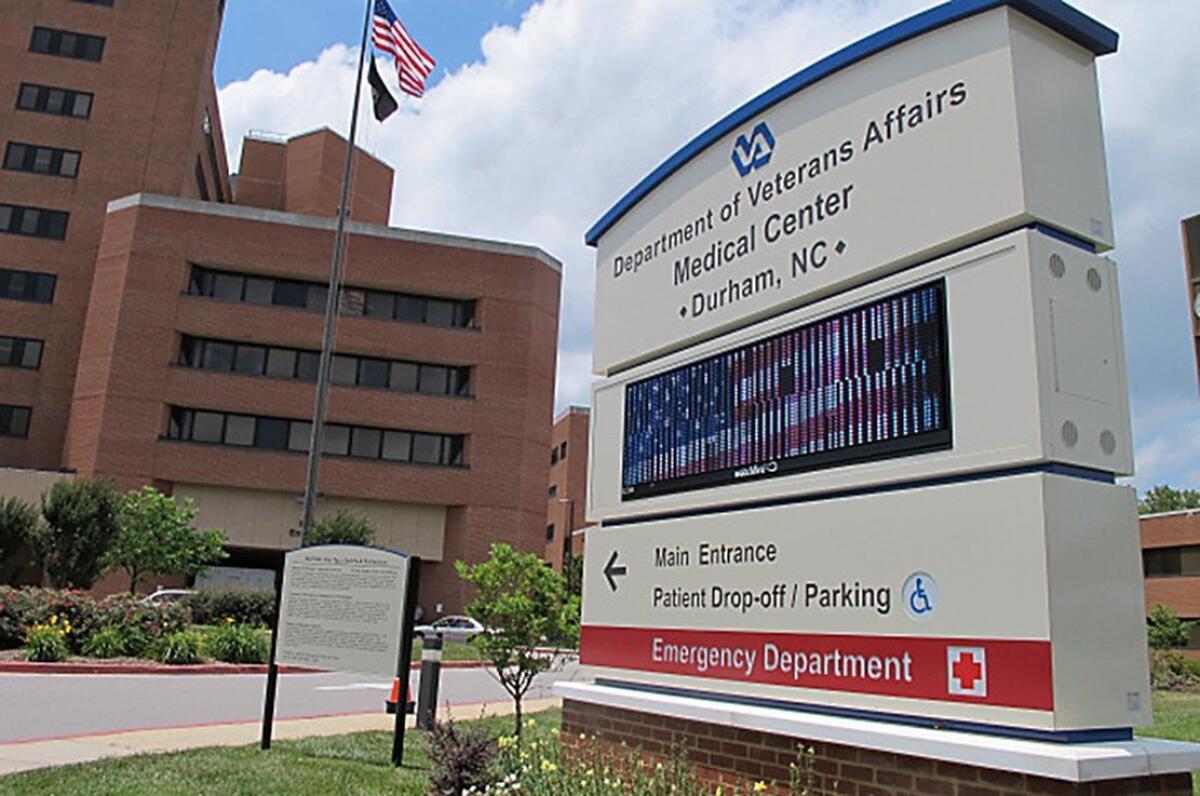
It turns out there is such a system: the U.S. Department of Veterans Affairs. And a new analysis of nearly 3.1 million patients in the VA system has found a different kind of racial divide: Blacks do significantly better than whites.
Over a nine-year period, researchers found that the adjusted mortality rate of African Americans was 24% lower than that of whites, according to a study published this month in the journal Circulation.
“We thought we were going to show they do the same if the same care is offered to both groups,” said senior author Dr. Kamyar Kalantar-Zadeh, a nephrologist and epidemiologist at UC Irvine. “But we found blacks do even better.
“This is a paradox within a paradox,” he said.
The results suggest that blacks may have genetic or other biological advantages that make them healthier than whites in some ways, but that those advantages are canceled out by other factors in society at large, the study authors wrote.
That idea is not new. Among patients with kidney disease, blacks survive longer than whites — a well-known exception to the overall pattern. Kidney care also happens to be an area of medicine without large racial disparities, since the U.S. government has long covered dialysis for anybody who needs it.
Kalantar-Zadeh and his colleagues wondered whether there were similar differences among people without kidney disease who had equal access to healthcare.
Using VA records, they identified 547,441 black patients and 2,525,525 white patients who had a normal kidney function test between 2004 and 2006. Most were men, and their average age was 60. The researchers tracked them for an average of eight years.
NEWSLETTER: Get the day’s top headlines from Times Editor Davan Maharaj >>
More than 638,000 died by the time the study period ended in July 2013. The annual mortality rate for white men was 31.9 per 1,000, compared with 22.5 per 1,000 for black men.
In part, that difference could be explained by the fact that the black population was six years younger on average. But after a statistical analysis taking into account a wide variety of factors — including age, gender, income, education, blood pressure, medications and body mass index — blacks were still far less likely to die during the study period.
African American men and women were also 37% less likely than white men to develop heart disease, the leading cause of death in the U.S. The researchers found no racial difference in the rate of strokes.
For comparison, the researchers conducted a similar analysis using six years of data from the National Health and Nutrition Examination Survey, a government study of about 5,000 people each year who are selected as a representative sample of the U.S. population.
In that analysis, the adjusted death rate was 42% higher for blacks than for whites.
In an editorial that accompanied the study in Circulation, Drs. Nakela Cook and George Mensah of the National Institutes of Health said the results raise important questions about health disparities in the U.S. They also cautioned that though there may be biological differences between blacks and whites, other factors could be at work as well.
For instance, they wrote, blacks in the VA system might have better underlying health than blacks in the general population — a gap that may be less pronounced for whites. Exercise, diet and other factors not considered in the study could also play a role.
And though the VA offers open-access healthcare to all veterans who qualify, there may be racial differences in how treatment is provided.
Follow me on Twitter @AlanZarembo and “like” Los Angeles Times Science & Health on Facebook.
MORE SCIENCE COVERAGE
When it comes to controlling weight, not all fruits and vegetables are created equal
Dinosaur discovery in Alaska: A duck-billed herbivore that didn’t fear the snow
Sex after heart attack: Enjoy without anxiety (but don’t count it as exercise)







