UCLA Ordered to Halt Cancer Drug Tests in ’85
- Share via
Federal health authorities, citing dozens of violations of safety rules governing experimental drug trials, banned UCLA cancer researchers from treating additional patients with such drugs for a 16-month period in 1985 and 1986, The Times has learned.
The violations included unauthorized distribution and use of drugs, inadequate evidence of patients’ consent to the drug therapy, improperly documented case histories and inadequate records on patients’ response to the drugs, according to documents obtained by The Times. Federal officials cited no instances in which patients were harmed because of negligence.
The suspension was ended July 3, 1986, when UCLA officials completed a reorganization of the system used to keep track of experimental drugs and to monitor their use on patients. UCLA never publicly announced the suspension, nor were patients who were already in the program--and whose therapy was not curtailed by the federal action--informed of it.
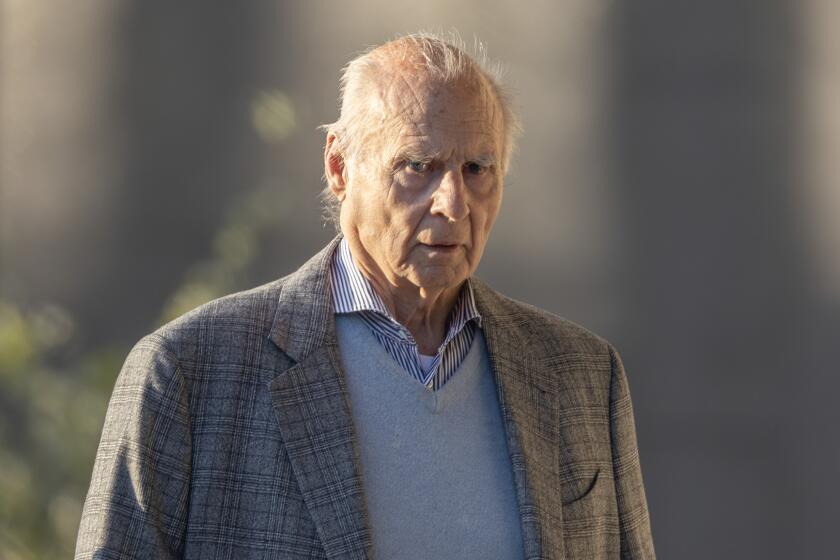
Among the researchers cited for violations were some of the university’s top cancer specialists, including Dr. Robert Gale, the physician who gained worldwide fame a year ago when he was invited to the Soviet Union to perform bone marrow transplants on victims of the Chernobyl nuclear plant disaster.
The suspension was imposed by the National Cancer Institute, which distributes drugs used in investigational therapy and keeps track of patients’ response. It followed inspections by the institute and the U.S. Food and Drug Administration, which is responsible for safeguarding patients in drug trials.
“There appeared to be a pervasive lack of knowledge or ignoring of the federal regulations relating to use of investigational agents,” the head of the cancer institute’s quality assurance and compliance section, Dr. Dorothy Macfarland, wrote in a March 19, 1985, letter to UCLA Vice Chancellor Albert Barber.
Dr. Frances O. Kelsey, director of the FDA’s division of scientific investigations, said her agency also found “many departures” from its regulations during the inspection.
Researchers were permitted to continue treatment of 382 patients already receiving the drugs at the time the suspension went into effect. The effect of the suspension was to prohibit physicians from taking any additional patients into the experimental drug program.
The National Cancer Institute is the world’s largest sponsor of clinical trials of drugs that are under investigation for their potential usefulness in treating cancer. Dozens of these drugs are being tested at any given time by physician-researchers at cancer treatment facilities across the nation. In addition to issuing the drugs to investigators, the institute is responsible for approving the details--known as protocols--of how the drug is to be tested and the adequacy of the record-keeping.
The FDA’s responsibility is to ensure that patient safety is maintained and to check the completeness and accuracy of the data recorded by the researchers.
Qualifying for License
The information obtained by the researchers is used to help the government decide whether a drug is worthy of being licensed for widespread use, so accurate and up-to-date records on patients’ reactions to the drugs are crucial.
Macfarland said in an interview that UCLA was one of five of the “hundreds” of inspected cancer centers in the nation to receive such a suspension and that the 16 months was the longest suspension enforced so far.
Officials at UCLA-Jonsson Cancer Center and the researchers characterize the violations identified by the government principally as paper work problems rather than substantive issues of patient care, but they note that they have complied with recommended changes in procedure.
Federal officials agree that the problems have been corrected and have no complaints about the researchers’ current conduct.
Team of Experts
The violations were uncovered by 10 experts from the institute, the FDA and other organizations who spent six weeks during March and April of 1985 at the medical center, digging through scores of boxes of records and speaking with each of the researchers.
The auditors found that investigational drugs received from the institute had been diverted to studies not approved by the institute, borrowed by unauthorized doctors for use on patients not in studies approved by the institute and distributed to physicians outside UCLA without monitoring by the responsible UCLA investigator.
In some cases, the diverted drugs were distributed to unauthorized physicians who wished to use them on their own patients who were not responding to other therapies. Such diversion, often called “compassionate use,” is allowed with institute approval, but in the UCLA cases the institute was not informed.
Inadequate Case Histories
In addition, inspectors said that some patients’ files lacked adequate case histories or a properly signed and witnessed informed consent form. In other cases, patients’ records failed to contain documentation of the treatment, the progress of the disease during treatment or an evaluation of the patient’s response to the drug he or she was receiving.
The violations primarily involved six faculty members who at the time were testing experimental drugs on patients with melanoma, osteosarcoma, neuroblastoma and adult leukemia. In addition to Gale, the physicians were Gregory Sarna, Andrew Jacobs, Robert Seeger, Richard Champlin and Frederick Eilber.
Gale was accused by the FDA of failing to provide the inspectors with his records of the use of an investigational drug for leukemia, which the FDA said had been improperly distributed to physicians outside the cancer center.
Not Told of Inspection
According to Gale, he had not been told that an inspection was scheduled until the day before and did not have enough time to retrieve the documents from storage and prepare them for the inspectors.
“Nobody had bothered to tell me that they (the inspectors) were coming,” Gale said in an interview. He said he provided FDA inspectors with the records at a subsequent visit to his office.
Sarna, director of the Bowyer Multidisciplinary Oncology Clinic, where outpatients receive anti-cancer drugs, said he is “not aware of any patient getting a drug that he or she shouldn’t have received or of receiving a drug inappropriately.”
He said the investigation had “correctly” identified a small number of incidents involving improperly transcribed or filed information and one case of a missing informed consent form.
Not Considered Significant
“Although the report appears to show several problem areas, a careful examination of the records suggests that the deficiencies are quantitatively fewer and qualitatively less significant than the report indicates,” Sarna said in a letter addressed to Dr. James Ruckle, the cancer center’s deputy director.
Similarly, the other researchers said they regarded their violations of federal regulations as primarily being administrative problems rather than “matters of substance.”
Dr. Richard Steckel, director of the cancer center, claimed in an interview that the center has been blamed for what he said was the National Cancer Institute’s “failure” to develop an adequate system of monitoring drugs to make sure they were being used appropriately.
He also complained that the facility had in effect taken the punishment for transgressions outside its jurisdiction. He noted that before the inspections, the institute dealt directly with the UCLA researchers--not with the cancer center’s administration--concerning new investigational drugs.
“But,” he said, “it is the cancer center that has been faulted for not dealing with the problem.”
Decision Defended
Steckel also defended the decision not to mention the suspension to patients already in the program and those who had not been directly affected by the suspension.
“We felt that no harm had been done, and we saw no reason to alarm anyone,” Steckel said. When the suspension was terminated on July 3, 1986, all six researchers and the cancer center were again authorized to conduct drug trials. That authorization, however, came only after UCLA officials had convinced the agency that it had established safeguards to prevent future violations.
Among these safeguards was the establishment of a central pharmacy that is the sole source of all National Cancer Institute investigational drugs dispensed to researchers. In order to obtain the drugs, investigators must comply with a number of restrictions intended to make sure that the investigator has met all institute and FDA requirements.
These restrictions include having on file at the pharmacy a copy of the approval of each study by the university’s Human Subjects Committee, which rules on legal, ethical and safety issues for every study involving patients. The pharmacy has been given full authority to refuse to dispense an investigational drug if the patient does not meet these and other eligibility requirements.
Accurate Records Needed
The investigator must certify that the drug will be administered only to subjects under his or her personal supervision or that of other doctors responsible to him. He must also agree to keep accurate records.
The safeguards prohibit researchers from diverting drugs without the approval of the National Cancer Institute to a doctor for the treatment of a patient who is not in the study but whom the doctor believes the drug will benefit.
Under the previous system, researchers in the program obtained about half their experimental drugs directly from the institute and half from the campus pharmacy.
Macfarland, the institute official who also was a member of the team that inspected UCLA, admitted that until 1983 a system for monitoring cancer drug trials was “non-existent.” But, she said, although the proper methods for keeping track of drugs were sent to UCLA in 1983, they were still not in place two years later at the time of the inspection.
Correcting the Problems
“Although we are dealing with a (monitoring) system that is evolving, once we find problems at a facility, we feel that they must be corrected at once,” she said.
“We feel that if a facility is going to go by the name of ‘cancer center,’ it ought to be responsible for the research taking place within its walls.”
Since the early 1980s, cancer researchers have been aware that the FDA was unhappy with the cancer institute’s monitoring methods and was trying to “whip NCI into shape” by pressuring it to tighten its system.
Dr. Alan Lisook, chief of the FDA’s clinical investigations branch, confirmed the agency’s displeasure with the institute and said the FDA began putting pressure on it to conduct tougher inspections beginning about five years ago. He said the FDA was concerned because the kind of drug data it often got from institute-sponsored trials was “useless” for determining the drug’s efficacy and whether it should be licensed.
He said the FDA was--and to a degree still is--concerned about the “sloppy” manner in which some cancer drug researchers maintain patient records.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.