COLUMN ONE : Faith Lost, a Doctor Turns Bitter : A drug used as an animal dewormer is also found to help treat cancer. Its price jumps--for cancer patients. A key researcher feels betrayed. But the maker says it’s only recovering its costs.
- Share via
ROCHESTER, Minn. — In more ways than one, it was an act of faith for Dr. Charles Moertel to rise, late in the morning on Sept. 28, 1989, before a dozen people seated around a National Cancer Institute conference table in Rockville, Md.
The cautious Mayo Clinic cancer researcher, a former president of the American Society of Clinical Oncology, had come to the NCI to describe a set of extraordinary test results. In a federally funded $11-million study of nearly 1,300 patients who’d undergone surgery to remove cancerous colon tissue, Moertel’s team had reduced recurrence of the disease by 41%, and the overall death rate by 33%, among those with advanced Stage C cancer. They’d done this, incredibly, with a therapy that combined levamisole, which has been used for 30 years to rid farm animals of worms, and fluorouracil, a widely used but not terribly effective chemotherapy drug.
By instinct a skeptical physician, reluctant to endorse new drugs not clearly proven safe and effective, Moertel for once felt convinced enough to go along with what others were urging. This therapy, he agreed, should be provided at once to certain colon cancer patients, even before the Food and Drug Administration granted formal approval.
Moertel’s faith in his science was matched by a trust in his audience. He was at the NCI, after all, to hand over his test results to officials from Johnson & Johnson, the giant $12-billion-a-year health care company that markets--and holds the patent on--levamisole. He was also there to offer Johnson & Johnson his considerable influence in winning FDA approval for this new combination therapy.
“I will do everything I can to help get this treatment to patients,” Moertel told the NCI, FDA and Johnson & Johnson people sitting before him. “I will appear before the FDA myself to speed up the approval process. In return, I ask only one thing. All I want is a promise from Johnson & Johnson that you will market this at a reasonable price.”
Looking back, there are those, of course, who would call Moertel’s stance a bit naive. After all, over the last decade prices for prescription drugs have risen nearly three times as quickly as other consumer prices. Drug companies’ average profit margin of 15.5% is more than triple the average of all Fortune 500 companies. Pharmaceuticals didn’t lead all United States industries in profitability in 1990 by letting Mayo Clinic professors decide what is a “reasonable” price for their drugs.
Nonetheless, Moertel left the NCI meeting that morning four years ago with his faith in science and drug companies intact. He believed he’d secured Johnson & Johnson’s promise.
“They definitely, unequivocally promised levamisole would be reasonably priced,” he recalled later. “I believed their assurances. I assumed they were honest and honorable people.”
Not until nine months later did Moertel learn that Johnson & Johnson--its new FDA approval in hand--had increased the price of levamisole a hundredfold. Marketed as an animal dewormer, levamisole costs 6 cents a pill; marketed as a cancer drug, it costs $6. Where a year’s supply costs $15 for a sheep, the same amount--150 milligrams a day--costs $1,200 for a human.
As Johnson & Johnson executives explained it, they were finally recovering their 25 years of research costs; as Moertel saw it, they were taking advantage of a captive market.
“I was amazed when I heard,” Moertel said recently. “I couldn’t believe it. This fell a little short of my definition of reasonable.”
So began the transformation of a trusting Mayo Clinic researcher into an outraged, outspoken industry critic.
Johnson & Johnson sees matters differently. “We disagree with Dr. Moertel. . . . We firmly believe that this price is fair and reasonable and that we are acting in the public interest,” said F. Robert Kniffin, the company’s vice president for external communications.
But for Charles Moertel, the story of levamisole, as richly revealing a portrait of the drug industry as any, has become an unceasing battle cry.
The Wonder Drug
The Belgian physician and researcher Paul A. J. Janssen had lofty goals when he set out, in the early 1960s, to find a superior treatment for parasite infestation in animals. He wanted a drug that was potent, safe, economical, injectable and active against a wide variety of larvae and worms.
In levamisole, he found just what he was after. Here was a fast-acting and quickly metabolized drug, effective in all sorts of animals, wild and domestic. By 1965, it was being marketed in Belgium. A year later, it was in Brazil. Soon, it was everywhere.
Levamisole gradually revolutionized agriculture, becoming the most widely used worm remedy in the world for cattle, pigs, sheep and poultry. It also became a popular dewormer for people; Johnson & Johnson, which had acquired Janssen Pharmaceutica in 1961, vigorously marketed levamisole for human use in Third World countries.
“For a while, it was the gold standard,” said Moertel. “It was a huge income source.”
As time went by, Paul Janssen began to hear intriguing reports about unexpected side effects. It looked as if levamisole was doing more than killing worms.
Pre-weaning mortality of beagle pups in Belgium fell from 25% to 5% when the bitches were given levamisole before whelping. Resistance of cattle in Chad to contagious bovine plueropneumonia increased noticeably. Sheep in South Africa experienced a striking decrease of chlamydial infections. The weight of “poor-doing” calves and pigs in Australia suddenly normalized.
Most veterinarians tended to attribute these effects to levamisole’s impact on the larval stages of worms. The larvae were thought to decrease resistance, so their elimination would naturally restore it.
But Janssen couldn’t avoid speculating: Might levamisole be a wonder drug? Might levamisole somehow be boosting immune systems? Might levamisole even be an effective anti-cancer drug?
In 1971, clinical studies began to test levamisole’s effect on myriad diseases--rheumatoid arthritis, multiple sclerosis, chronic hepatitis, herpes, Crohn’s disease. In 1972, Janssen and Johnson & Johnson filed their first application with the U.S. Patent Office, seeking a sweeping patent on levamisole as an aid in the “regression and palliation” of virtually all tumors--”neoplastic disease”--whatever their nature and location.
“Drug research is like an orchestra . . . “ Janssen wrote soon after in a journal article about levamisole’s development. “Creative thinking cannot but suffocate in a world of bureaucratic materialism where ideals cannot be realized and beautiful dreams can no longer come true. . . . Superior drugs, designed to meet essential health needs, will not be found or even recognized by the complacent, unimaginative and lazy-minded. . . . “
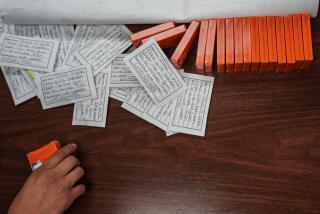
Be they unimaginative and lazy-minded, or merely dubious of unproven claims, Patent Office examiners weren’t buying what Janssen’s group had to offer. The patent file for levamisole as a cancer drug involves a half-foot-high, 13-year-long pile of petitions, rejections, appeals, refilings and more rejections. Between 1972 and 1985, eight separate or amended applications were turned down.
“Neoplastic disease” was “too broad and indefinite” a definition of what the drug treats, the examiner ruled repeatedly. What’s more, “there is insufficient evidence” that the drug is “safe and effective.”
By the early 1980s, the patent applications were specifying types of cancers--breast, lung, colon--and offering a summary of 26 levamisole studies worldwide. Still, the Patent Office was not impressed. In 1983, an examiner remained of the opinion that “there is insufficient evidence . . . demonstrating (that) the applicants’ compound is effective for treating cancer in humans.”
One problem, according to Moertel, was that “the studies of levamisole were pretty junky. Some would come along and say, ‘Whoopee.’ Others would say, ‘No, it doesn’t help, it even hurts.’ There were funny results. . . . Evidence for therapeutic benefit has almost invariably failed the test of confirmation.”
Moertel heard about one such study in early 1978, while attending a conference in Bethesda, Md. In a test involving 60 patients with advanced Stage C colon cancer (the type that has spread to nearby lymph nodes), a Belgian researcher named Herman Verhaegen was reporting a distinct survival advantage for the 30 who’d received levamisole after surgery.
Moertel wasn’t overly impressed, for Verhaegen’s work involved quite a small group. What’s more, although Verhaegen had made it sound like a truly randomized test--a “placebo-controlled” trial, he’d called it--the patients in fact had not been randomly assigned to the levamisole or placebo groups. Verhaegen had decided which patients would get the levamisole. By doing so, he could easily have skewed the results.
Still, Moertel was interested. Three years before, he’d gathered a number of upper Midwest community clinics together and formed the North Central Cancer Treatment Group, with him and the Mayo Clinic as consultants. Colon cancer was precisely what this group was seeing over and over, in places like St. Cloud and Fargo and Duluth. Nationwide, colon cancer was second only to lung cancer as the leading cause of cancer-related deaths. Colon cancer afflicted more than 100,000 Americans a year, and caused 54,000 deaths. In the advanced Stage C type, cancer recurred in about half of the 21,000 patients who underwent surgery each year.
It would be a good idea for our group to test levamisole, Moertel reasoned. Even if it didn’t work, it would establish our testing procedures and quality control.
Because levamisole’s credentials as a stand-alone cancer drug weren’t impressive, Moertel decided to combine it with the chemotherapy drug fluorouracil, commonly known as 5-FU. In use for 25 years, 5-FU’s impact had been limited--some tumors shrank, some relapses were delayed, that was all--but Moertel thought the drugs just might work in tandem.
He began with a small pilot group of Mayo Clinic patients with incurable colon cancer to reduce chances of unusual side effects. When none were apparent, he launched a first-phase study of 401 colon cancer patients throughout the upper Midwest. One randomly selected group received levamisole after surgery, one group no treatment, and one group levamisole combined with 5-FU.
Three years into the study, it became apparent that the levamisole alone was having virtually no effect. But it also became apparent that the combination of levamisole and 5-FU was significantly delaying or stopping the return of cancer in advanced Stage C patients.
“By 1984, we were saying, ‘Hey, this is something we haven’t seen befo” Moertel recalled. “The study wasn’t over, but it looked very interesting.”
In January, 1985, with full NCI funding, a larger, nationwide, 1,300-patient second-phase trial began under Moertel’s supervision. Johnson & Johnson supplied the levamisole for free, but otherwise played no role in the test. “We had no contact with them,” said Moertel. “There was no communication.”
Johnson & Johnson, all the same, was in motion. The pharmaceutical concern had never given up trying to get a patent on levamisole as a cancer drug. After providing the Patent Office only with an article summarizing 26 levamisole studies, the company finally delivered the actual studies.
All had been conducted before 1980, and none had been followed up with more contemporary experiments. In 1992, a scientific review of levamisole in the “Biologic Therapy of Cancer” would describe pre-1980 levamisole studies as “inconclusive or negative” and “relatively unsophisticated.”
In early 1984, however, the Patent Office examiner who’d been denying the levamisole applications for a dozen years apparently found the 26 articles’ cumulative weight persuasive. Relenting, he finally granted most of Janssen’s claims. In June, 1985, an appeals board allowed the others.
The patent on levamisole itself had expired months before and couldn’t be renewed. But on April 22, 1986, Janssen Pharmaceutica was granted what’s called a “use patent,” which gave it the exclusive right to market levamisole as a “process of aiding regression and palliation of neoplastic disease in animal and human hosts.”
Johnson & Johnson still didn’t have the type of convincing proof required for Food and Drug Administration approval to market a new drug; the FDA was a much higher hurdle than the Patent Office. So three years passed without Johnson & Johnson filing an application to use levamisole as a cancer drug.
Then, one day in the summer of 1989, the drug company received a felicitous phone call from someone inside the National Cancer Institute. The NCI official had good news. A team of Mayo Clinic cancer researchers, it seemed, had just come up with precisely what Johnson & Johnson so urgently needed.
Result So Clear
When drafting the protocol for his large second-phase study, Moertel had written a provision saying they’d report their results early if they looked extremely good or bad during interim analyses. To reach that threshold, however, would take quite a lot, for Moertel was notoriously conservative.
Time and again over the years, his colleagues saw breakthroughs where he saw only a dreadful price being paid in side effects, expense and dashed hopes. Sometimes, he took public positions. He organized the government-sponsored study that discredited Laetrile as a cancer cure. He challenged Nobel Prize-winning chemist Linus Pauling’s claim of large doses of Vitamin C as a cancer cure. He wrote a scathing medical journal editorial questioning the worth of the immune system booster interlukin-2. He warned about the overhyping of the cancer drug interferon.
All the same, by the spring of 1989 it was clear even to Moertel: Levamisole and 5-FU in combination were substantially reducing recurrence of colon cancer.
In June, 1989, he called the FDA. Preparations soon began to arrange for doctors to get levamisole from the NCI, under certain rules, before the FDA approved it for marketing.
The next step was to secure FDA approval. This was the responsibility not of the Mayo Clinic or the NCI, but of the levamisole patent-holder--Johnson & Johnson. (5-FU already had FDA approval; no longer under patent, it is sold by several companies.)
“Who else could have filed an application?” Moertel asked recently. “I guess I could have. It’s not my business to make money on drugs, though. I don’t care if the drug company makes money off my work. I get paid a nice salary. And I’m doing something good for folks. I have a nice home, and I’m going fishing this weekend. What more do I need?”
Contacted by the NCI, representatives from Johnson & Johnson met Moertel, FDA and NCI officials in Rockville in September, 1989. It was here that Moertel sought--and thought he’d secured--Johnson & Johnson’s promise to market levamisole at “a reasonable cost.”
On Oct. 2, at an NCI press conference and in a Journal of Clinical Oncology article, Moertel’s team announced the results of their Phase I study. Until the FDA cleared levamisole for commercial sale as a cancer treatment, the NCI advised, it would be provided to doctors on a free, experimental basis. When it is cleared for sale, said a spokeswoman for Janssen Pharmaceutica, the drug would be “reasonably priced.”
Two weeks later, the NCI gave the company the data tapes from Moertel’s study. On Oct. 31, Janssen Research Foundation filed a new drug application with the FDA. On Feb. 1, 1990, Moertel--having paid for his hotel and airfare to avoid any accusations of conflict--made a presentation on Johnson & Johnson’s behalf before the FDA’s oncologic drug advisory committee, a group he’d previously sat on for 13 years. On Feb. 8, Moertel’s report of his large Phase II study appeared in the New England Journal of Medicine. On June 18, the FDA gave Janssen approval to market levamisole as a cancer treatment in combination with 5-FU.
A process that on average takes drug companies 2 1/2 years had, with Moertel’s endorsement, taken six months.
“It’s hard to say what I would have done if I hadn’t been assured about the pricing,” Moertel said later. “They could have gotten the approval on their own; it just wouldn’t have been as easy or quick or cheap. And my main interest was to get this on the market quickly. My main interest was to save lives.”
Doctor Storms Around
One morning in late September, 1990, a 77-year-old farm woman named Annie Rhymes stopped by her drugstore in Rockport, Ill., to fill a prescription for her post-operative colon cancer treatment. She gasped when she learned a bottle of levamisole would cost $200.
After all, down the road from the pharmacy, at the local Farm & Fleet store, a comparable bottle of levamisole intended for sheep was priced at $6.39.
When Rhymes raised the matter with her physician, he too was taken aback. Dr. Merickston Nicholson knew Rhymes couldn’t afford $200. He also believed the pills over at the Farm & Fleet were the same drug, only a larger dose; according to Moertel at the Mayo Clinic, they had different inert fillers, but were manufactured to federal standards as rigid as the FDA’s. If Rhymes were of a mind to, she could buy her pills at the Farm & Fleet, break them up, and take half a pill three times a day.
Nicholson thought this situation was ridiculous. He also thought it merited public attention, so he called the local newspaper. A day later, a reporter for the Rockford Register called the Mayo Clinic. Moertel erupted when the reporter told him the news.
He began to “storm around,” as he later put it. He provided the reporter with a string of angry quotes. He protested to Johnson & Johnson sales representatives. He spoke out during appearances before professional groups.
In time, Johnson & Johnson apparently grew concerned over such a public demonstration by a highly respected cancer researcher. One day, a company representative called Moertel from Johnson & Johnson headquarters in New Brunswick, N. J. Could they fly out to the Mayo Clinic to discuss this matter? Soon, two Johnson & Johnson vice presidents were in Moertel’s office, spreading out their graphics.
“They talked about all the money they’d put into basic research,” Moertel recalled. “Then they showed me charts with three price-structuring options. The first, $400 for a year’s supply of levamisole, covered profit, marketing and research, even though the taxpayers actually paid for (our) research. The second and third options, $800 and $1,200 for a year’s supply, covered no additional research or profit; it was all for more promotion.”
Moertel understood perfectly why the vice presidents assumed these charts would please and mollify him. Many of those extra promotional dollars attached to the $1,200 annual price tag, after all, would go to doctors and hospitals.
Most marketing by drug companies is aimed not at the consumer, but at the medical community that writes the prescriptions. This marketing often comes camouflaged as educational and research grants. Increasingly, health economists say, drug companies are hiring doctors as “consultants,” and sponsoring conferences, and offering “contributions” to clinics and nonprofit hospitals.
Those who study such matters believe drug makers spend about $12 billion annually on marketing and promotion--about $1 billion more than they do on research and development. Educated estimates vary, since the industry will not reveal precise figures, but Stephen W. Schondelmeyer, a professor of pharmaceutical management at the University of Minnesota, says a typical drug company spends 16% of its budget on research and development and 20% on promotion.
Watching this trend build in recent years, Moertel has grown ever more dismayed. Doctors have always been offered a box of golf balls or doughnuts, but now there are enormous amounts of money on the table. Now every medical group Moertel knows is taking drug company money.
More than once, Moertel himself has received overtures. One drug firm wanted to give the North Central Cancer Treatment Group $80,000 with no strings attached and no tie-in to the company’s products. To Moertel, this was not research and development money, this was drug company “marketing.” He turned it down.
The promotion chunk of Johnson & Johnson’s levamisole pricing chart looked to Moertel to be nothing more than giving money to doctors and clinics.
“They didn’t have to promote levamisole,” he said. “They had extraordinary publicity, and taxpayer-paid research. In essence, they were promoting Johnson & Johnson, not the drug. They were cultivating goodwill by putting money into doctors’ pockets. I was not pleased. The patients have to pay in the end. We doctors can pay for our own continuing education.”
For a while, Moertel still hung back, reluctant to push the matter further. When the CBS show “60 Minutes” came calling, he declined. Moertel hoped the matter could be resolved privately.
There was no resolution, however. Instead, Moertel watched Johnson & Johnson continue to spend promotional money.
The company, according to Moertel, asked a Mayo Clinic colleague to be a consultant on an “educational program” for doctors, and ended up paying him $4,000 for editing four sentences that were already written. Other Mayo colleagues, Moertel reported, were provided free airline tickets, hotel rooms and honorariums to “edit” an already prepared slide show.
“Johnson & Johnson also followed me around,” Moertel said. “They’d show up at conferences where I was talking. For a while, they were chasing me around with money. I couldn’t get away from it. I was scheduled to speak at a Scripps conference in San Diego. Johnson & Johnson went to the Scripps people and said they wanted to make a donation, they wanted to pay for the cost of Moertel’s participation. When I learned of this, I refused to go if they were paying.”
Moertel’s brushes with Johnson & Johnson, in time, set him to stewing more generally about the pharmaceutical industry.
He’d frequently heard drug companies argue that their high profitability was justified because theirs is a high-risk business. We spend an average of $231 million and 12 years to bring each new drug to market, they’d always point out, and only one of 5,000 compounds tested results in an FDA-approved drug. Without high returns, there’d be no incentive for innovative, risky research. Without high returns, there’d be fewer drugs that save lives and reduce the ruinous cost of surgery.
Although these arguments undeniably carried some weight in the medical community and on Capitol Hill, Moertel by now had little patience with such talk. It would be easier to accept the drug companies’ arguments, Moertel felt, if they didn’t spend more on promotion than research, and didn’t pour an average 58% of their research money into “me too drugs” that duplicate what’s already on the market, and didn’t benefit so greatly from the taxpayer-financed work of academic and federal researchers. NCI-funded scientists alone, Moertel knew, had played key roles in developing 70 cancer drugs being marketed by private companies.
The last straw for the Mayo Clinic professor came when he learned that a year’s supply of levamisole in Europe--marketed as a cancer treatment, not a dewormer--was going to average $150, one-eighth of the cost in America. “American consumers are supporting research and development for the world,” he fumed. “They’re tough over there in Europe and we’re pussycats. We’re the only Western nation that doesn’t regulate drug prices. This is out of hand. This is nonsense.”
In the spring of 1992--after his levamisole study was formally completed, after he was convinced they had a treatment that truly worked--Moertel decided to go public with his grievances.
He looked at his calender. The annual meeting of the American Society of Clinical Oncology was coming up in San Diego in May. He was scheduled to speak at the plenary session, where he’d submit his final study results. That would be the best forum, he decided. That’s where he’d make a public fuss.
On May 19 at the San Diego Convention Center, before an audience of 5,000 doctors and a couple of national news cameras, Moertel devoted most of his talk to his study’s final results. Then, near the end, he added two or three lines about levamisole’s cost.
The pricing was “unconscionable,” he said. “We were specifically promised that it would be marketed at a reasonable price. . . . I’d think after 25 years of profitable marketing, they’d more than made up their costs. The National Cancer Institute, funded by the American taxpayer, sponsored this study. . . . The company got a present dumped in its lap. We gave it to them on a silver platter.”
At least implicitly, Moertel was pointing a finger not just at Johnson & Johnson, but also at those of his colleagues who help keep drug prices high by accepting the pharmaceutical industry’s “promotional” dollars. So he wasn’t sure what kind of response he’d get.
What he got was a loud, huge, sustained ovation. Afterward, many from the audience approached Moertel to congratulate him. You’re right, I agree, what can we do? they kept asking.
“Make the Johnson & Johnson-Janssen booth here the loneliest place in town,” Moertel suggested.
Company Holds Firm
A flurry of newspaper articles followed Moertel’s speech. So did an appearance on the ABC-TV program “PrimeTime Live.”
As a result, several colon cancer patients came forward to say they decided to take the sheep version of levamisole, even though Johnson & Johnson--differing with Moertel--warned that it is “totally unsuitable for human consumption.”
Soon, levamisole was regularly being invoked in the continuing national debate over drug company pricing and health care reform. In Chicago, after watching Moertel on TV in the summer of 1992, Frank Glickman, a 47-year-old real estate business consultant who’d recently undergone colon cancer surgery and levamisole/5-FU treatment, filed a class-action lawsuit challenging Johnson & Johnson’s patent on levamisole and seeking damages for the drug company’s “unconscionable and outrageously excessive price.”
In the face of such aggressive responses, Johnson & Johnson so far has held firm.
The annual $1,250 cost of levamisole “is less than the average cost of one day’s confinement in a hospital in the United States . . . “ observed Johnson & Johnson spokesman Kniffin in a written statement. “Among available cancer drugs, Ergamisol (the company’s brand name for levamisole) is very modestly priced. . . . For patients deemed financially unable to pay, we have maintained an indigent patient program that provides Ergamisol free of charge. . . . Over a period of some 25 years, more than 1,400 costly studies involving over 40,000 patients were completed. . . . It was this work, including tens of millions of dollars of research investment made by our company, that led to a study funded by the National Cancer Institute that showed the effectiveness of levamisole. . . . Profits from the sale of Ergamisol . . . will probably never cover the cost of our total investment in research and development for this compound for human use.”
Although equally resolute, Johnson & Johnson’s reply to Frank Glickman’s lawsuit--which is still in the preliminary-motion stage--sounded a somewhat different theme. Rather than mention “research costs” or “indigent programs,” the drug company’s legal brief focused mainly on the monopoly rights of a patent holder.
“Whatever (its) merits, (Glickman) cannot bring this lawsuit . . . “ the drug company’s memorandum of law argued. “Patentees are given the right to charge whatever price the market will bear for their patented products. . . . (This) freedom . . . is a right deliberately given by the federal government to patent owners in order to reward them for their useful inventions that improve our society. . . . Glickman’s complaint is . . . a complaint about federal patent policy itself. As such, it may be remedied--if at all--only in the Congress, not in this court.”
Johnson & Johnson probably is right. The courts generally have not supported attacks on what is, finally, a monopoly granted under federal patent law. In late July, two generic drug firms that were challenging the Burroughs Wellcome Co.’s patent on the anti-AIDS drug AZT--because federal money and researchers played a key role in its development--lost their battle when a federal judge decided he could “no longer find a legal basis for the case.”
If changes are to come, they probably must be fashioned--as Johnson & Johnson suggests--in Congress. Whether that will happen is unclear.
Over the years, Congress has made frequent but usually fruitless efforts to regulate the drug industry. In 1990, a Senate committee held hearings on the industry’s promotional activities, and in 1991 the FDA tried to limit some “continuing education” promotional efforts, but these efforts faltered in the face of negative pressure from the American Medical Assn. So did reform bills introduced in November, 1991, by Sen. David Pryor (D-Ark.) and Rep. Pete Stark (D-Oakland).
Talk still mounts about regulating the pharmaceutical industry as governments do utility monopolies, or letting any company market a drug if it pays a royalty to the patent holder. But Moertel’s by-now thoroughly impassioned battle cry--”We need a price control system, and this business about levamisole shows why”--will face tough challenges when a health care reform package goes to Capitol Hill.
A Mystery Lingers
The particular resolution to the levamisole story, at any rate, may very well come from the laboratories of the Mayo Clinic rather than from the halls of Congress. After all, there’s still a lingering mystery about levamisole waiting to be solved. There’s still an unanswered question about the true medical value of Johnson & Johnson’s drug.
Leading scientists now agree that levamisole--by itself--has utterly no effect on cancer. Earlier studies that suggested otherwise--the earlier studies that helped Johnson & Johnson win a patent in 1986--have been soundly refuted in more recent trials.
“Treatment with levamisole alone had no detectable effect,” Moertel reported in his February, 1990, New England Journal of Medicine article. “Our study and (another) recently reported trial . . . provide convincing evidence that levamisole alone is of little or no value in patients with colon cancer.”
Scientists simply aren’t sure why the combination of levamisole and 5-FU works. Some think levamisole enhances 5-FU’s effect by boosting the patient’s immune system. Some think levamisole and 5-FU may undergo a biochemical reaction when combined. And some think levamisole doesn’t do anything at all.
In an editorial published alongside Moertel’s study in the New England Journal of Medicine, Dr. Robert J. Mayer of the Dana-Farber Cancer Institute in Boston wrote: “It is possible . . . that the observed effect of (5-FU) combined with levamisole may be attributable to (5-FU) alone, perhaps administered with better compliance among patients than (in) previous trials.” Studies show 5-FU “may also be enhanced” by folinic acid. This combination “might prove to be far more effective” than 5-FU and levamisole. Which combination is best “remains to be determined.”
The laws of nature, in other words, might yet prove a greater influence on levamisole’s price than the laws of Congress or the U.S. Patent Office. Levamisole’s greatest value might yet turn out to be as a wondrous--and inexpensive--dewormer for humans and farm animals all over the world.