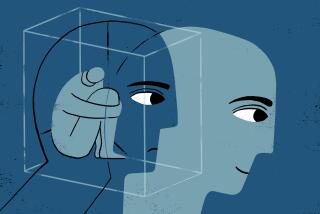
Mild Depression Common and Harmful, Study Finds
- Share via
One out of nine Los Angeles residents endures mild depression that is pronounced enough to affect their jobs and families, according to a study of a newly recognized malaise that falls in the diagnostic gray zone between having a clinical disorder and having a bad day.
The survey of 2,393 adults was part of an ongoing national study to gauge how many people feel depressed and yet would not be labeled with major depression. The work focuses on an experimental and controversial category in the psychological menu of misery known as “subsyndromal depression.”
The new study is a “significant contribution to understanding mood disorders,” said Dr. Victor Reus, a psychiatrist at the UC San Francisco School of Medicine. It shows that “the categories we’ve had so far don’t include all the individuals who have been suffering from depressive symptoms,” he said.
Now, psychiatrists diagnose people as depressed if, for no obvious reason such as a loved one’s death, they experience at least five of nine general symptoms for two weeks: deep sadness, apathy, fatigue, agitation, sleep disturbances, weight or appetite change, lack of concentration, feelings of worthlessness and morbid thoughts.
Subsyndromal depression, or SSD, the researchers say, is a milder version, marked by the otherwise inexplicable appearance of two to four of those symptoms for two weeks. SSD is not included in the latest edition of the standard psychiatric diagnostic manual.
“People who have some depression symptoms have nearly as much disability [at work and home] as do people with major depression,” said Dr. Kenneth Wells, a psychiatrist at UCLA Medical School and the Rand Corp. and a coauthor of the study. It appears today in the American Journal of Psychiatry.
In the Los Angeles survey, mental health workers visited randomly selected Hispanic and non-Hispanic whites and conducted interviews in Spanish or English. They found that 270 people, or 11.2%, had SSD, while 102, or 4.3%, had major depression. Those figures are in line with surveys conducted in St. Louis and Durham, N.C., the two other cities studied.
As expected, people with the subthreshold syndrome reported more household strain, more financial pressure and more days spent sick in bed than did people without depression. In addition, subsyndromal depression appeared to affect many areas of daily life almost as much as did the full-fledged clinical disorder.
In both groups, roughly 60% said that in the previous month they had had fewer than 13 “social contacts”--visits or talks with friends or loved ones not in the same household. And compared with the clinically depressed, slightly more in the subsyndromal group (62%) were said to have “high social irritability,” meaning they were upset or angry with loved ones or co-workers more than once a month.
The findings underscore the view that depression is not a singular disease entity, but instead encompasses a range of symptoms of varying intensity, Wells said. He added that research is underway to determine whether counseling or drug therapy might help people with subsyndromal depression. “If treatment matters even a modest amount, it could have large public implications because there are so many people with this problem,” he said.
Some researchers, however, worry that this new category of mood disorder, which was first suggested by UCLA’s Wells in a 1989 study, may be seized upon by drug companies before there is convincing evidence that drug therapy works. “It’s clearly of concern if this enlarges the market share of the pharmaceutical industry,” UC San Franciso’s Reus said.
And others see the new work as part of a trend toward defining all bad habits as addictions and all forms of despair as disease.
“This seems to be part of the continuing effort by the psychiatric establishment to expand into everyday life and define it in terms of medical conditions,” said Stanton Peele, a social psychologist in Morristown, N.J., and author of “The Diseasing of America.”
The study’s lead author, Dr. Lewis Judd, a UC San Diego psychiatrist and former director of the National Institute of Mental Health, acknowledged that the work was controversial. “People are concerned about trying to make an illness out of what looks to be life’s normal ups and downs,” he said.
He added that some of the resistance to expanding the scope of depression reflected the long-standing stigma against mental disease. “If we found that the threshold for high blood pressure was lower than what everybody thought in the past,” he said, “it would not be an issue.”
“I’m certain that the everyday waxing and waning of the human spirit is a normal phenomenon that most of us experience across life,” he said. “However, if you have a consistent cluster of depressive symptoms that persist for weeks, that may be a serious problem, even though it doesn’t meet the clinical definition of depression.
“This is not a benign condition,” Judd said of subthreshold depression. “It’s worthy of clinical attention.”