A Bacterial Link May Make IBS Responsive to Antibiotics
- Share via
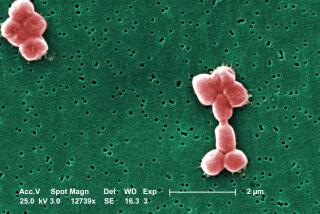
Irritable bowel syndrome, a gastrointestinal disorder characterized by bloating, abdominal pain and diarrhea or constipation, may be caused in some cases by an overgrowth of intestinal bacteria and may be cured with antibiotics, according to researchers from Cedars-Sinai Medical Center in Los Angeles.
The disorder afflicts as many as 20% of the adult U.S. population, striking twice as many women as men, and there is currently no good treatment available.
Dr. Mark Pimentel and his colleagues evaluated 202 IBS patients using a special breath test to determine the presence of bacterial overgrowth in the small intestine. They reported in the December issue of the American Journal of Gastroenterology that bacterial overgrowth was present in 78% of them. They then treated those who tested positive with a 10-day course of antibiotics.
Forty-seven of those patients returned for a follow-up breath test. The Cedars team found no bacterial overgrowth in 25 and reduced overgrowth in 22. Among the 25 with no overgrowth, 12 had no symptoms of IBS whatsoever and the remaining 13 had sharply reduced symptoms. Symptoms were also reduced in those patients who showed only partial eradication of the overgrowth. Pimentel suggested that a different regimen of antibiotics might help the latter group. The team has now begun a larger, controlled trial of the antibiotic therapy.
Last month, a new IBS drug called Lotronex was pulled from the market because it was linked to a bowel condition called ischemic colitis, which restricts blood flow to the colon. Three deaths may have been caused by the drug. Another new IBS drug called Zelmac is expected to be approved by the Food and Drug Administration soon.
Compulsive Buyers Respond to Medication
A small preliminary test has found that a new drug called citalopram can help control a behavior disorder called compulsive shopping.
Compulsive shopping, which actually is compulsive buying, is an impulse-control disorder that is often associated with depression. It is estimated that 2% to 8% of the U.S. population, most of them women, suffers from the problem.
Dr. Lorrin Koran and colleagues at the Stanford University Medical School gave the drug, trade-named Celexa, to 19 women and two men. They reported at an American College of Neuropsychopharmacology meeting in Puerto Rico that 80% of the subjects showed a positive response. The patients exhibited less anxiety, less depression and less impulsiveness.
“The women in the study reported they stopped thinking about shopping,” Koran said. The group is now beginning a larger study in which the patients will not know whether they receive the drug or a placebo.
Study Rejects Calcium as a Nail Strengthener
Women who take calcium supplements to strengthen their nails are wasting their money, according to a study in the Dec. 14 New England Journal of Medicine.
Dr. Ian R. Reid of the University of Auckland in New Zealand studied 683 women who had taken calcium supplements or placebo tablets in an osteoporosis study. Reid’s team queried the women about their nail strength and concluded that those taking calcium received no benefit. Reid said that the belief that calcium improves nail strength is widespread but noted that bones have 800 times more calcium than nails. Nails simply don’t need much calcium.
‘Mini Strokes’ Seem to Augur Larger Episodes
Transient ischemic attacks, so-called mini-strokes that pass quickly and leave no permanent damage, are often harbingers of more disastrous strokes and should receive prompt medical attention, according to a new study.
Dr. S. Claiborne Johnston and his colleagues at UC San Francisco studied 1,707 patients who had mini-strokes and reported in the Dec. 13 Journal of the American Medical Assn. that 180 had a stroke within three months after the event. That 10.5% rate is in line with previous research and was not unexpected. But they also found that half happened within two days of the initial mini-stroke. “No one expected that. That was a surprise,” Johnston said.
About 300,000 Americans have transient ischemic attacks each year. Symptoms include sudden numbness and blurred vision but disappear within 15 minutes to 24 hours and don’t cause permanent damage. The new findings indicate patients need to be seen by a doctor immediately and that the problem should be taken very seriously, Johnston said.
Breast Cancer Battle May Have a New Drug
A large international study has found that a new drug called Femara may be somewhat better at fighting advanced breast cancer than tamoxifen, the currently used treatment.
In a study of 907 postmenopausal women with advanced breast cancer, researchers found that Femara provided a median of 3.6 more months before cancers worsened than did tamoxifen, researchers told a Food and Drug Administration advisory committee last week. That is a significant improvement for such severe cases. Overall, the risk of the disease worsening was 30% less in the Femara patients than in the tamoxifen patients.
Novartis Pharmaceuticals Corp., which sponsored the study, already sells Femara for use when tamoxifen treatment fails. In light of the new results, the FDA may upgrade its approval so that Femara is the first drug used in treatment.
Drug Tests Well on One Form of Dementia
A new drug called rivastigmine may significantly reduce the symptoms of a common form of dementia called dementia with Lewy bodies.
Accounting for 15% to 25% of all cases of dementia, this form is characterized by fluctuating impairment in thinking ability, attention deficits, visual hallucinations and Parkinson’s-like symptoms. There is currently no effective treatment for it, and its cause is unknown.
An international team headed by Dr. Ian McKeith of the University of Newcastle upon Tyne in the United Kingdom studied 120 patients with dementia with Lewy bodies in the United Kingdom, Spain and Italy. Half received rivastigmine and half a placebo.
The team reported in the Dec. 16 issue of Lancet that patients taking rivastigmine were significantly less apathetic and anxious and had fewer delusions and hallucinations. At least a 30% improvement in symptoms was shown by 63% of those taking rivastigmine, compared with only 30% of those taking placebo. The principal side effects include gastrointestinal disturbances and weight loss.
*
Medical writer Thomas H. Maugh II can be reached at thomas.maugh@latimes.com. Capsules runs every Monday.