A way to choose a baby’s gender
- Share via
Once they decided to have children, MiShel and Carl Meissner tackled the next big issue: Should they try to have a girl?
It was no small matter. MiShel’s brother had become blind from a hereditary condition in his early 20s, and the Meissners had learned that the condition is a disorder passed from mothers to sons. If they had a boy, he would have a 50% chance of having the condition. A girl would be unaffected.
The New Hampshire couple’s inquiries about gender selection led them in 1999 to Fairfax, Va., where a new sperm-separation technique, called MicroSort, was under investigation. The couple’s first attempt at artificial insemination, using sperm sorted by sex chromosome, was a failure. But on the second attempt a few months later, MiShel became pregnant and gave birth to a daughter. They will try to have a second daughter using the technique later this year.
“I probably would not have had children if not for MicroSort,” she said. “This was pretty much our only option for kids.”
The technique separates sperm into two groups -- those that carry the X-chromosome (which leads to a female baby) and those that carry the Y-chromosome (which produces a male baby). The process was developed in the early 1990s by the Genetics & IVF Institute in Fairfax, and last week’s opening of a MicroSort laboratory in Laguna Hills marks the company’s first expansion.
“We believe the number of people who want this technology is greater than those who have access to it,” said Dr. Keith L. Blauer, the company’s clinical director.
The expansion brings with it not only a seemingly effective way to select a child’s gender -- it also highlights a host of ethical and practical considerations that accompany sex selection, especially for the majority of families who use the technique for nonmedical reasons.
The Laguna Hills clinic, which is a joint effort with the Huntington Reproductive Center of Southern California, offers sex selection for two purposes: to help couples avoid passing on a gender-linked genetic disease and to allow families who already have a child of one gender “balance” their families by having a baby of the opposite sex. (More than 500 X-linked diseases, such as Duchenne muscular dystrophy and hemophilia, are passed from mothers to sons.)
The technology is still experimental; couples using the method will do so as part of a clinical trial overseen by the Food and Drug Administration. However, Blauer says the company has impressive success rates; 91% of the women who become pregnant after sorting for a girl are successful, while 76% who sort for a boy and get pregnant are successful. Couples hoping for a girl are nine times more likely to get a girl compared with natural selection, while those desiring a boy increase chances by threefold.
Fertility experts agree that the technique is significantly different from other sex-selection methods, some of which they describe as little more than “voodoo.” They include sex-selection diets (eating salty foods supposedly increases the chances of having a boy), an ancient Chinese birth calendar that suggests timing conception to a particular time of the year and the more common sperm-spinning methods that many infertility clinics offer today. The spinning technique uses centrifugal force to try to separate sperm. But most doctors say the method is hardly better than the 50-50 chance nature provides.
“The success rates for these other methods are not good,” said Dr. Larry Lipshultz, a professor of urology at the Baylor College of Medicine, in Houston. “They are very comparable to flipping a coin.”
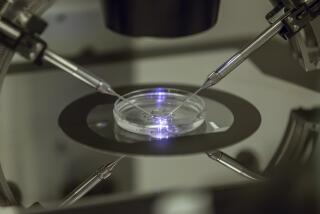
The new technique separates sperm based on the fact that the X chromosome is larger than the Y chromosome. A machine is used to distinguish the size differences and sort the sperm accordingly. The result is then checked using another type of DNA analysis to ensure that it contains mostly X- or Y-bearing sperm. The desired sample is then used for artificial insemination or in-vitro fertilization.
But even this gender-selection process is not as accurate as a post-conception technique called pre-implantation genetic diagnosis. In that, doctors create embryos using in-vitro fertilization. A cell is then removed from each embryo and analyzed for genetic characteristics before selected embryos are implanted in the woman’s uterus.
Pre-implantation genetic diagnosis is highly accurate when determining gender or the presence of genetic disease, but it is costly and poses ethical dilemmas for some couples.
The Meissners ruled out less scientific approaches as unreliable and were uncomfortable with pre-implantation genetic diagnosis, because that method creates embryos that would go unused, something the couple was uneasy about. “If another person would choose to do pre-implantation genetic diagnosis, fine. But I didn’t think I could do it,” MiShel Meissner said. “It’s a very personal choice.”
While the Meissners wished to avoid passing on a genetic disease, 86% of the MicroSort’s clients so far have used the method for “family balancing,” with most of them seeking girls.
It’s the idea of choosing a baby’s gender for personal satisfaction that is most controversial. England forbids the use of preconception sex selection for nonmedical reasons, and the governing body for infertility specialists in the U.S. frowned on the practice until 2001, when the group softened its stance.
The American Society for Reproductive Medicine’s new position reflects changing attitudes about technology as people become more comfortable with it, says Dr. Daniel A. Potter, medical director of MicroSort’s West Coast center. Some couples, he adds, will keep having babies naturally, trying to get the gender they desire, a behavior that also raises ethical questions.
“When you have new technology, there will always be questions. But this is technology that couples can use, so they won’t use methods that don’t work,” Potter said. Still, some reproductive health doctors will not perform sex selection for nonmedical reasons, said Susan Benoff, president of the Society for Male Reproduction and Urology.
And, said Lipshultz, “It’s also a question of utilizing resources that could be best used for couples who can’t have any children at all. Some people question whether doctors should be spending their time on that.”
MicroSort officials, however, said their goal is to establish the method’s safety, efficacy and cost-effectiveness so that it becomes “a routine part of family planning.”
Right now, MicroSort costs $2,300 plus fees for artificial insemination, which are usually about $200. (Under the clinical trials protocol, the company is waiving fees for couples who use the technique to avoid passing on an inherited disease.)
Pre-implantation genetic diagnosis requires in-vitro fertilization, which can cost $10,000 or more per cycle. The new technique can also be used with in-vitro fertilization, which greatly increases its price. Using artificial insemination, couples have a 15% to 20% chance of pregnancy per attempt compared to an IVF pregnancy success rate of about 25% per attempt.
“For people who really want to do this, using pre-implantation genetic diagnosis is the more secure way to go” because of its near-100% accuracy and higher pregnancy rate, said Dr. Richard Paulson, an infertility specialist at USC. “I wonder if PGD will end up being more cost-effective.”
According to Paulson, doctors have questioned whether the sperm-sorting technique can provide a large enough sample to ensure a decent chance of pregnancy. A typical sample contains 3 million to 5 million sperm. But after going through sorting, the sample size is usually about 200,000 to 300,000 sperm, which, Blauer concedes, has traditionally been viewed as too small to produce a good chance at pregnancy via insemination.
However, the company has gathered data showing that the sample is large enough to maintain pregnancy rates that equal nature’s, he said. That data will be presented later this year at a meeting of the Pacific Coast Reproductive Society.
The company needs 364 live births but needs 750 plus follow-up safety and efficacy data before it can request that the FDA approve the technology. Blauer predicts the clinical trial will be completed in about two years -- an accelerated schedule now that the company has two MicroSort labs in operation.
*
Seek counseling
Couples who want to choose the gender of their baby for nonmedical reasons should first have counseling, says the American Society of Reproductive Medicine. It should ensure that they:
* Know the risk of failure.
* Can fully accept children of the opposite sex if the procedure fails.
* Don’t have unrealistic behavior expectations for the preferred gender.
* Are offered the chance to participate in research to track the safety, efficacy and demographics of preconception gender selection.