Researchers use stem cells to rein in Type 1 diabetes
- Share via
Researchers have demonstrated for the first time that the progression of Type 1 diabetes can be halted -- and possibly reversed -- by a stem-cell transplant that preserves the body’s diminishing ability to make insulin, according to a study published today.
The experimental therapy eliminated the need for insulin injections for months or even years in 14 of 15 patients recently diagnosed with the disease. One subject, a 30-year-old male, hasn’t taken insulin since his stem-cell transplant more than three years ago, according to the study in the Journal of the American Medical Assn.
The study suggests a new avenue for treating the intractable disease, in which the immune system destroys insulin-producing beta cells in the pancreas. Without insulin, patients can’t metabolize sugar and run the risk of developing nerve damage, cardiovascular disease, kidney failure and blindness.
Patients with Type 1 diabetes typically compensate by monitoring their blood-sugar levels every few hours and injecting themselves with insulin as many as five times a day.
After the stem-cell treatment, “patients are absolutely medication-free -- they’re off insulin,” said Dr. Richard Burt, chief of the Division of Immunotherapy for Autoimmune Diseases at Northwestern University’s Feinberg School of Medicine in Chicago and senior author of the study.
The strategy is similar to an approach that has shown some success in treating other immune system disorders, such as rheumatoid arthritis, lupus and multiple sclerosis.
“We all realize that without addressing the problem at the level of the immune system, we’ll never really beat Type 1 diabetes,” said Dr. Francisco Prieto, who treats diabetics in his Elk Grove, Calif., practice and wasn’t involved in the study. “This is very encouraging work.”
Burt and his colleagues cautioned that they didn’t know whether the fix was permanent and, if it was not, how long it would last. One of the subjects was insulin-free for one year but relapsed after a respiratory viral infection, said lead author Dr. Julio Voltarelli, associate professor of medicine at Ribeirao Preto medical school at the University of Sao Paulo in Brazil.
The researchers also cautioned that the process was not without risk, because patients are vulnerable to infection during part of the therapy. Burt’s research group at Northwestern has performed 170 stem-cell transplants to treat a variety of immune system disorders, and two patients have died from the treatment.
But other doctors said that even if the benefits of the therapy were temporary, the research provided valuable insight into the mechanism behind the disease.
“It’s a big deal,” said Dr. Stephen Forman, chairman of the Division of Hematology & Hematopoietic Cell Transplantation at the City of Hope Comprehensive Cancer Center in Duarte, who wasn’t part of the study. “The fact that you got somebody insulin-independent, there’s a clue there” for scientists in search of a cure.
The Juvenile Diabetes Research Foundation in New York estimates that as many as 3 million Americans have Type 1 diabetes, and that 30,000 to 35,000 new cases are diagnosed each year.
Most of those patients will die from complications of the disease rather than from diabetes itself. The age of onset is considerably younger than for patients with Type 2 diabetes, who can still make insulin but can’t use it efficiently.
The stem-cell approach mirrors the bone marrow transplants used to treat patients with certain cancers and blood diseases.
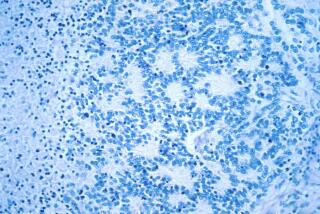
Bone marrow contains hematopoietic stem cells, which are able to build all of the elements of the immune system. The idea is to wipe out the faulty immune system and replace it with a new one that functions properly.
In the study, 15 Brazilian patients were treated within a few months of their diagnoses, before their immune systems had the chance to eradicate all of their insulin-producing cells. The researchers hoped to preserve enough beta cells to make insulin injections unnecessary.
The study was conducted in Brazil because of Voltarelli’s interest in the experiment. It was funded by the Brazilian Ministry of Health and other sources.
The patients, ages 14 to 31, were treated with drugs and hormones that prompted the body to produce hematopoietic stem cells and send them from the bone marrow into the bloodstream, from which a machine then extracted them.
About two weeks later, the patients checked into the hospital and received chemotherapy and other drugs to kill off their immune systems over a period of five days. Side effects for most patients included nausea, vomiting and hair loss.
After a day of rest, they were infused with their own hematopoietic stem cells, which took about eight to 12 days to establish new immune systems. While the patients were without functioning immune systems, they were given antibiotics to protect them from possible infections.
The treatment had no effect on the first patient, whose disease had progressed so that his blood was dangerously acidic. He also took steroids to help him tolerate some of the drugs.
After the patient’s poor results, the researchers modified the study’s protocol to exclude patients with his condition, called diabetic ketoacidosis, and to remove the steroids from the drug regimen.
Of the remaining 14 patients, 12 were able to stop taking insulin shortly after their transplants. Five patients have not needed insulin injections for at least 23 months, and two have been insulin-free for more than a year and a half.
One patient relapsed seven days after her transplant but gradually reduced her insulin dosage and was able to stop her injections after one year. Another patient became insulin-free 20 months after her transplant.
Voltarelli said he wasn’t sure why two patients had a delayed response to the transplants.
“Maybe their immune systems took more time to recover and stop destroying the pancreatic” beta cells, he said.
Dr. Defu Zeng, a diabetes researcher at City of Hope, has used a similar technique to wean diabetic mice off insulin. All of the mice eventually relapsed, which leads him to suspect that the Brazilian diabetics will too.
“We need to wait at least five or six years,” Zeng said. “It’s too early to make any conclusions.”
Even if patients continue to require insulin shots, the treatment should be considered a success if it halts the destruction of beta cells, said Dr. Jay S. Skyler, associate director of the Diabetes Research Institute at the University of Miami’s Miller School of Medicine, who wrote an editorial accompanying the study.
Retaining at least some insulin-producing cells makes the disease easier to control and less likely to result in severe complications, like blindness.
Patients who were diagnosed with Type 1 diabetes long ago would not benefit from a stem-cell transplant because their immune systems have left nothing to preserve, he said.
Some of those patients are now treated with transplants of beta cells harvested from cadavers. Scientists also are trying to use embryonic stem cells to grow beta cells for transplant.
In the long term, the treatment could potentially be combined with beta cell transplants to help patients who don’t have any of their own beta cells left.
If the research ultimately leads to a therapy, Prieto predicted that patients would embrace it despite the risks inherent in destroying one’s immune system.
“If you ask any patient with Type 1 diabetes, would they go through tremendous hardship and trials in order to be free of insulin shots, most of them would tell you yes,” said Prieto, who serves on the Independent Citizens’ Oversight Committee of the California Institute for Regenerative Medicine.
“The risk that you could go into ketoacidosis and not survive -- that’s real. It happens every day.”
*
(BEGIN TEXT OF INFOBOX)
A new strategy for Type 1 diabetes
--
Patients develop Type 1 diabetes when their immune systems attack cells in the pancreas that produce insulin. An experimental technique involving stem-cell transplants allowed 14 out of 15 patients with Type 1 diabetes to stop their insulin injections. Here’s how it works:
* Hematopoietic stem cells, which can create a new immune system, are harvested from the patient’s blood.
* Chemotherapy and other drugs are used to destroy the patient’s faulty immune system.
* The stem cells are transplanted back into the patient to establish a new immune system that doesn’t attack pancreatic cells.
--
Source: Times staff reporting