New hope for celiac disease sufferers?
- Share via
In a sense, the 2 million plus Americans with celiac disease are lucky. No other autoimmune disease has such a safe and effective treatment.
Purging the diet of gluten -- the protein in wheat, rye and barley that triggers an immune reaction in the gut -- can reverse the disease and reduce intestinal inflammation. That’s important, because studies now show that the consequences of untreated celiac disease are graver than previously thought, causing anemia, arthritis, osteoporosis, hepatitis, neurological problems and even malignancies, as well as increased general mortality.
Still, it is very difficult to eliminate gluten entirely. It lurks in disparate sources such as vinegars, soy sauce, medications, lip balm and Play-Doh (which some children consider edible); and even gluten-free foods, which are expensive, may contain enough traces to cause symptoms. “When we study celiac patients who have been doing their best to follow a gluten-free diet, even after five years we see lots of damage in the small intestines in about half of them,” said Dr. Robert Anderson, a gastroenterologist in Melbourne, Australia, who is working on a vaccine to prevent or switch off the reaction to gluten.
His is one of many efforts underway to develop new, non-dietary treatments for celiac disease. Ultimately, celiac patients may be able to take a pill before a meal so they could, for example, have stuffing with their holiday turkey. Or, as is Anderson’s goal, they could go for a series of treatments similar to allergy shots that would teach their immune systems to tolerate gluten.
“It’s very exciting that the pathophysiology of celiac disease is understood to such a degree that we can design potential therapies,” said Dr. Peter Green, director of the Celiac Disease Center at Columbia University College of Physicians and Surgeons in New York.
There are two categories of treatments being developed. One would supplement a gluten-free diet and protect patients from occasional gluten exposure; the other would train the immune system to tolerate gluten and allow patients to eat a regular diet.
Enzyme therapy
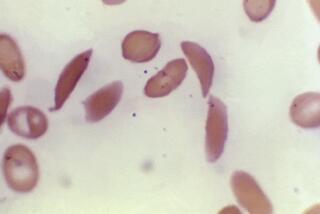
Within the first category, one approach uses oral enzymes that target gluten. We cannot completely digest gluten because humans lack digestive enzymes that can break it down, but researchers at Stanford University combined enzymes from bacteria and barley that finish what our own digestive juices cannot. They showed in rats that when gluten is broken down into smaller fragments, it no longer causes inflammation in the intestines. Alvine Pharmaceuticals, based in San Carlos, Calif., has developed this “glutenase” therapy and is now recruiting patients for a Phase II clinical trial.
In this trial, as with the others, participants have had a diagnosis of celiac disease confirmed by a biopsy but have had it under control on a gluten-free diet. They are given either a drug or placebo, along with a gluten challenge, often the equivalent of one or two slices of bread.
“From the early data it looks like the oral enzymes break down enough gluten to be useful,” said Dr. Daniel Leffler, director of clinical research for the Celiac Center at Beth Israel Deaconess Medical Center in Boston. Leffler was not involved in the enzyme trial but is an investigator in a nearly completed Phase II trial testing a different drug, larazotide, developed by Alba Therapeutics in Maryland.
The larazotide approach leaves the gluten peptides, or small fragments of proteins,intact but aims to prevent them from penetrating beneath the lining of the gut into the mucous layer where the immune reaction occurs. In celiac disease, as in many autoimmune diseases, including Type 1 diabetes, this intestinal barrier is “leaky” or permeable.
Larazotide is a bioengineered drug designed to close those leaks to keep out gluten and prevent or reverse the disease. In preliminary results from about 300 patients in Phase I and II trials, the drug did seem to benefit patients, who had fewer adverse symptoms after eating gluten. It also reduced the levels of the antibody that serves as a blood marker for the immune response to gluten. But interestingly, the drug did not seem to reduce intestinal permeability.
“So the drug works, but maybe through a different mechanism that we don’t understand yet,” said Green, who is on the clinical advisory board for both Alba and Alvine. He predicts that, if ultimately found effective, the oral enzymes and larazotide would be marketed as supplements to a gluten-free diet but that many patients would want them to actually replace the restrictive diet. It’s unclear not only whether such a use would be possible but also whether it would be a daily regimen or followed only when dining out or traveling, for instance.
Immunotherapy
The second category of treatment, known as immunotherapy, is more investigational but also more exciting, Leffler said. It would allow patients to eat a regular diet by quelling immune response in the gut. This response is driven by immune cells known as T cells, which react when other immune cells display gluten fragments on their surface.
In Australia, a company founded by Anderson, called Nexpep, is packaging the gluten peptides that trigger this immune response into a vaccine that will desensitize the immune reaction. The theory, which he says works in animals, is that by introducing these peptides through injections under the skin rather than through the gut, the immune cells learn to tolerate them and no longer display them to the T cells. That can theoretically prevent or turn off the reaction that damages the intestines
Anderson expects Phase I safety trials of this vaccine, Nexvax2, to be completed in mid-2010. He anticipates that patients would receive a series of injections of the vaccine, followed by occasional maintenance doses.
“If we can figure out how to give the drug, how frequently and when we need maintenance therapy,” he added, “then we can use the same principle to explore treatments for other autoimmune diseases.” Several other groups are also developing vaccines for celiac disease, but this one is furthest along.
A low-tech immunotherapy approach might require just one inoculation -- of hookworm. It is known that a non-pathogenic hookworm introduced to the gut can relieve asthma symptoms. Researchers suspect that it is because we evolved with intestinal parasites that trained our immune system to tolerate environmental irritants, but our hygienic modern living has deprived us of this beneficial symbiosis.
Researchers at the Brisbane Princess Alexandra Hospital in Queensland, Australia, tested the effects of hookworm inoculation on 20 patients with celiac disease to see if it would blunt the immune response to gluten. In addition to hoping to provide relief for celiac patients, the researchers want to learn if this could be an effective therapy for inflammatory bowel disease and Crohn’s disease.
The results have not been published, but when the Phase II trial was over and the patients were offered a medication that would kill the parasites, they all opted to keep their hookworms.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.