Why isn’t more COVID-19 vaccine available immediately?

- Share via
To truly control the pandemic, most people around the world need to be vaccinated against COVID-19. That’s a tall order involving billions of shots.
By the end of this year, only about 70 million doses of the COVID-19 vaccines from Pfizer and BioNTech and from Moderna and the National Institutes of Health are expected to be shipped out worldwide. Next year, that number will jump to more than 1 billion. Other companies are also working on vaccines, but some populations still might not gain access until 2024.
In the meantime, the death toll continues to rise.
So why can’t doses be pumped out and distributed faster?
Considering that vaccines can take years just to create — and that Pfizer’s and Moderna’s vaccines went from concept to testing to deployment in less than a year — the pace is already swift.
Then there’s the issue of how many people need it: an amount unprecedented in the pharmaceutical industry.
COVID-19 vaccines are now being administered to healthcare workers in the U.S. What are your questions about the timeline, the safety or the science?
“We’ve never distributed vaccines on this scale before,” said Lois Privor-Dumm, director of adult vaccines at the International Vaccine Access Center at the Johns Hopkins Bloomberg School of Public Health. “We’re talking about trying to reach the whole planet, essentially.”
On the manufacturing side, there’s a hustle to expand production to more factories, which need to be fitted out with specialized equipment, and to train workers. And once made, Pfizer’s and Moderna’s vaccines must be kept at freezing temperatures, so they can’t be distributed in just any vehicle or stored in just any warehouse.
“It’s not like making widgets,” said Nancy Pire-Smerkanich, assistant professor of regulatory and quality sciences at the USC School of Pharmacy.
Instead of spending the time and money to build new factories to expand their capacity, pharmaceutical firms — including Pfizer and Moderna — are largely turning to contractors that specialize in vaccine manufacturing.
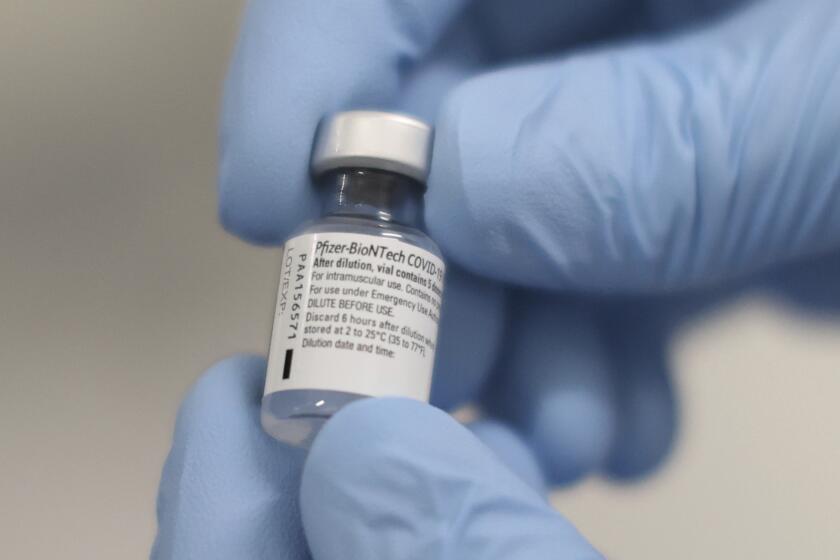
Pfizer is using several of its own factories in the U.S. and Belgium and is teaming up with outside companies to scale up manufacturing, a spokeswoman said. Moderna, whose business historically has not involved much production, is more reliant on third parties.
Developing vaccines can be a lengthy process, but the yearly flu vaccine is produced on a much shorter timescale than some other shots. That’s possible because all the technology has already been established — it’s only a matter of switching in the flu strains that researchers anticipate will be dominant that year, Pire-Smerkanich said.
The federal government has poured billions into COVID-19 vaccine research, but will Americans reap the profits?
For the 2020-2021 flu season, vaccine manufacturers expect to make up to 198 million doses for the U.S. alone, according to the Centers for Disease Control and Prevention.
Making COVID-19 vaccines is different: Manufacturers started from scratch, but they’re using a faster process.
The Pfizer and Moderna shots both use a technology called messenger RNA, or mRNA. Those molecules instruct cells how to make a specific type of protein that’s also found on the coronavirus, and this protein stimulates the immune system to make antibodies that would target the virus.
The mRNA technique speeds up the vaccine development process.
Many flu vaccines take about six months to make because they rely on growing the virus in chicken eggs. The mRNA technique, on the other hand, is developed in a lab and can be done much faster — in 2013, it took researchers at Novartis eight days to make a potential influenza vaccine.
This mRNA technology has been studied for decades, but no vaccine for humans has used the technique until now.
A major challenge for this technique is that the mRNA is fragile, which is why Pfizer and Moderna’s vaccines must be frozen. Pfizer’s vaccine must be kept at minus-94 degrees Fahrenheit; Moderna’s is more stable and can be stored at minus-4 degrees and last 30 days in a regular refrigerator. Both vaccines can keep for short periods of time outside of refrigeration.
The ultra-cold temperatures needed for Pfizer’s vaccine complicate the shipping process: Vials must be packed in freezer cases with dry ice, and a big shipment can contain more dry ice than is normally allowed on planes — a limit imposed because of the risk of carbon dioxide poisoning.
If production and shipping could be instantly ramped up, the bottleneck would be finding places for all those doses to be kept until use. Companies specializing in cold storage operations are now in high demand; L.A. County has acquired more than a dozen ultra-cold storage freezers to keep the vaccine before distribution. As it is, this need is likely to pose a problem in countries whose electric grids are less built out.
“If 90% of the world is not vaccinated, the virus will still be out there,” said Rhiju Das, an associate professor of biochemistry at Stanford University School of Medicine. “This really needs to be a worldwide immunization effort, otherwise COVID will be with us for a long time.”
Both vaccines require two doses, which means health systems will need to keep tabs on who has gotten the first shot and remind people to come back for the second, said Christopher Tang, a distinguished professor and chair in business administration at the UCLA Anderson School of Management.
And the process of making vaccines is specialized, involving equipment that is sometimes custom-made and workers trained in the raw materials, equipment operation, packaging and quality control. Every batch of vaccine is tested and inspected before the doses are sent out for distribution, and that all takes time.
“As much as we’ve automated the business, there’s still a level of expertise required when doing this,” Pire-Smerkanich said.
Experts say the speed of the process has been a major achievement.
In the world of vaccine development, failure rates are high, and makers often try multiple options before finding one that works, according to a May article in the New England Journal of Medicine.
And sometimes success comes too late.
For example, vaccine development for SARS and Zika was completed after both epidemics had ended, in 2003 and the mid-2010s, respectively. Federal agencies then reallocated the funds earmarked for that vaccine research, “leaving manufacturers with financial losses and setting back other vaccine-development programs,” according to the New England Journal of Medicine article.
In this case, vaccines have been created in time to play a crucial role in curbing the COVID-19 pandemic. Now it’s a matter of rolling them out.
“I don’t think we’ve seen anything quite on this scale,” said Eugene Schneller, a professor of supply-chain management at Arizona State University and a visiting scholar at the UCLA Fielding School of Public Health. “Although you’d like to have more ... I think we’ve done and are doing pretty well. The proof will be in the pudding of the consistency and quality of those vaccines as they come, and the integrity of the whole process.”
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.