Leaving prison for many means homelessness and overdose. California hopes to change that

- Share via
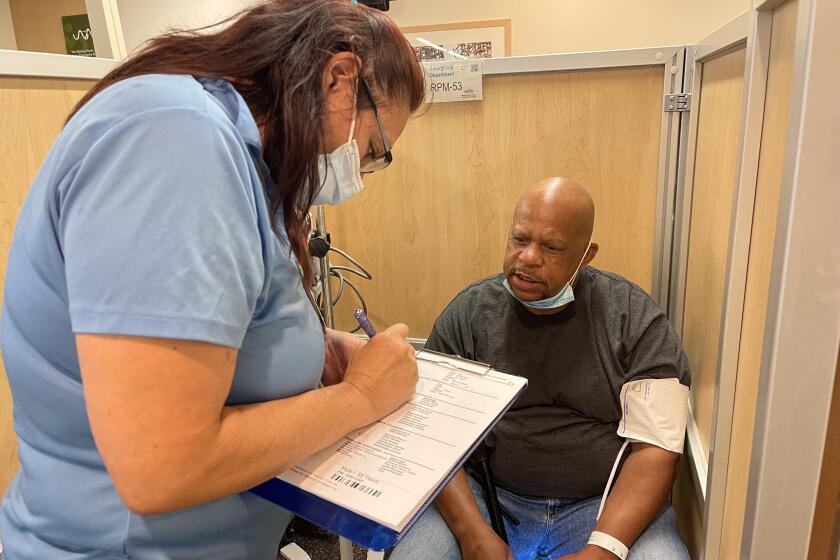
Lee Reed hoped that upon leaving prison he could return to the manual labor jobs he’d worked as a younger man.
But the 62-year-old suffered a debilitating back injury in prison, and despite requests for surgery, approval came only shortly before he was released, he said. It was too late. He would have to find a way to have the operation after getting out.
After 25 years behind bars for assault, Reed in July returned to a transformed San Francisco. Many of his loved ones were dead. He had no money or home. Depression settled in.
“I’m fighting myself, fighting the system, and I’m fighting to do paperwork, because it’s hard to get up to get around. I can barely move,” said Reed, who is living in a shelter.
Californians who leave prisons and jails soon will have a better chance of success beyond bars.
In January, California became the first state permitted to provide some benefits under Medicaid (known here as Medi-Cal) to incarcerated individuals. The new benefits would start 90 days before discharge in an effort to create a smooth transition to the community.
The Department of Health and Human Services approved the state’s request for a waiver of long-standing federal rules that prevented coverage of people behind bars.
Eligible enrollees include those who are pregnant or have mental illnesses, substance use disorders or chronic physical conditions and disabilities, as well as anyone in a juvenile facility.
“This is the first time in history Medicaid will be providing coverage to justice-involved individuals before they’re released,” Health Secretary Xavier Becerra said in a statement. “It is a step forward in closing gaps in services this under-served community experiences, and I encourage other states to follow California’s lead.”
After spending his life in and out of prison, Donald Winston landed his first apartment, thanks to a new California health insurance initiative.
Becerra said the Biden administration is focused “on expanding access to healthcare across the country and doing so with equity in mind” — a pledge that dovetails with the approval of California’s request.
Despite being a significant expansion of Medi-Cal and a break with past restrictions, the move has drawn support from corrections officials and conservative groups that more often oppose state spending programs. Some back the new policy because it means Washington will pick up part of the cost of inmate healthcare that is currently borne by state and local governments.
Medi-Cal is jointly paid for by the state and federal governments, with Washington covering about 65% of California’s Medicaid spending in the 2021 fiscal year.
“It’s always helpful to the state budget when California can draw down federal dollars,” said Susan Shelley, vice president of communications for the Howard Jarvis Taxpayers Assn., a nonprofit lobbying organization opposed to raising taxes.
Arizona, Montana, Utah, Kentucky and Vermont are among about a dozen states with pending proposals to similarly change their policies, and many believe California is blazing a path.
“Our goal is really to improve people’s health outcomes and behavioral health outcomes, as well as do it in a cost-effective way. And, if possible, change the trajectory of someone’s life,” said Jacey Cooper, California’s Medicaid director and chief deputy director of healthcare programs at the Department of Health Care Services.

Nearly $235 million is earmarked for the new initiative in the state’s proposed budget for 2023-24 — which equates to less than 0.2% of the roughly $139-billion total annual Medi-Cal spending.
The approved waiver also adds $410 million that correctional facilities, county behavioral health agencies and community-based providers will have available for planning efforts and developing infrastructure to implement the programs, said state healthcare officials.
Even those who support the experiment stress that its success will depend on how it is implemented.
Incarcerated people returning to the community face a slew of challenges, including life-threatening health risks. Stress surges as they seek to secure housing, find a job, access healthcare and reconnect to family and the fabric of social life. Many are simultaneously struggling with mental illness and drug addiction that are difficult to manage when there’s a gap in treatment.
The potential for peril is particularly acute in the period immediately after release. The risk of death in the first two weeks can be more than 12 times higher than in the general population, a 2007 study found — a grim statistic driven by drug overdoses, suicide, homicide and cardiovascular disease.
Hundreds of mentally ill detainees incarcerated across California in recent years have languished in jail long after being declared incompetent to stand trial.
Under California’s new policy, Medi-Cal will cover substance use treatment for eligible incarcerated people while they’re inside and connect them to a community-based provider before they are released so they can continue getting care, according to federal officials. It also allows for certain mental health interventions, including access to long-acting, injectable anti-psychotic medications.
As a condition of the approval, California is required to increase the amount it pays Medi-Cal providers for obstetrics and primary care. The state’s proposed budget allots roughly $22 million for the rate increases.
Prior to the approval, California rolled out reforms that didn’t require permission from the federal government.
Since the start of this year, anyone who enters a California jail, prison or juvenile facility must be screened and enrolled in Medi-Cal, if eligible; state officials estimate that encompasses 80% of the incarcerated population. The insurance is suspended while they’re behind bars but can be reinstated after release — or before, if they meet eligibility requirements.

Although the program has drawn praise, some experts and advocates worry that prison and jail officials will hold too much sway over the new benefits, pointing to what they say is often poor quality of healthcare in jails and prisons. Others fear it won’t be paired with adequate investment in other parts of the fractured health system — or will become a bureaucratic boondoggle.
“Just by having Medicaid existing inside these facilities doesn’t mean that, all of a sudden, jails and prisons are going to become this therapeutic space, but it does present the opportunity to improve the quality of care that is being placed there — because there’s oversight,” said Shannon Scully, senior manager of criminal justice policy at the National Alliance on Mental Illness, which supports fully eliminating the inmate exclusion policy.
Dr. Shira Shavit, executive director of Transitions Clinic Network, which is dedicated to reducing health disparities for individuals returning from incarceration, called the policy shift “a real moment for prevention.”
“If we intervene,” she said, “we can keep people out of the hospital, keep people from dying, but also keep them from going back to prison and jail.”
Kory Honea, president of the California State Sheriffs’ Assn., said success for the policy would depend on whether people take advantage of the new services.
“This is a challenging population to deal with,” he said. “If people have substance abuse issues or mental health issues, oftentimes, when they’re out of custody, they don’t avail themselves of the services or programs that you set up.”
Reed — who ostensibly would have been helped by the policy — remains skeptical that it will make a difference.
Before he left prison, Reed said, Social Security Administration employees in Kings County took his information to connect him with services. However, he said, they refused to transfer any of it to San Francisco, where he lives. (A spokesperson for the Social Security Administration said claims that are started during incarceration typically can be transferred to another office, but privacy laws prohibit discussion of Reed’s case.)

And with many employees in social services and corrections still working from home, Reed said he has felt alone as he tries to maneuver within labyrinthine care systems.
“I really want to break down and cry, but I ain’t got the time,” Reed said. “I just have to keep pushing.”
The California Department of Corrections and Rehabilitation, which operates state prisons, said in a statement that the plan “would provide releasing incarcerated individuals with access to critical healthcare resources in the community to ensure there is continuity of care upon release.”
Shavit said the “secret sauce” to successfully bringing incarcerated people back into the community is hiring those who have done time themselves for care teams. This approach provides a path to employment for the formerly incarcerated and offers hope in the neighborhoods where the teams work — often low-income communities of color with few resources, said Joe Calderon, who spent nearly two decades behind bars and now trains formerly incarcerated community healthcare workers at the Transitions Clinic Network.
“How can we save money, but more importantly, save lives and add quality of life to a community that’s historically been forgotten about?” Calderon said, adding that he sees California’s broader healthcare reforms as a step in the right direction.
MLK Community Hospital in South Los Angeles is surrounded by poverty and homeless encampments. Will Newsom’s health initiative improve access to care?
Change won’t happen overnight. It’s expected to take about three years to roll out the services across the state, starting with some county jails and juvenile facilities in April 2024, said Cooper, with the state Department of Health Care Services. The program is not expected to reach full maturity before the federal waiver ends in late 2026.
The state will need time to develop guidance and dole out money to build needed infrastructure, then wait for facilities to develop programs and assess whether they’re up to par. Not all of the programs will look the same, and they will launch in phases, Cooper said.
“This is a transformation,” Cooper said. “Transformation is a process; it’s not an event.”
- Share via
Watch L.A. Times Today at 7 p.m. on Spectrum News 1 on Channel 1 or live stream on the Spectrum News App. Palos Verdes Peninsula and Orange County viewers can watch on Cox Systems on channel 99.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.